| Citation: | Please cite this article as: Álvarezzaballos S, Zatarainnicolás E, Fernándezavilés F, Muñoz P, Martínezsellés M. Transcatheter aortic valve implantation used to treat active infective endocarditis with severe aortic regurgitation in an 88-year-old patient. J Geriatr Cardiol 2025; 22(3): 401−403. DOI: 10.26599/1671-5411.2025.03.003. |
Infective endocarditis (IE) remains a severe and life-threatening disease, with rising incidence and a particularly high mortality rate, especially among elderly patients.[1] While antibiotics are the mainstay of treatment, the success rate in left-sided IE is often limited, as nearly half of all patients eventually require surgical intervention for definitive management.[2] Heart failure is the main indication for surgery, but access to surgery is frequently restricted by several factors, particularly in patients with advanced age, often driven by the presence of comorbidities or hemodynamic instability.[3,4] Transcatheter aortic valve implantation (TAVI) is increasingly used to treat severe aortic stenosis but active infective endocarditis has been considered an absolute contraindication and data regarding the use of TAVI to treat aortic valve regurgitation are scarce.[5,6]
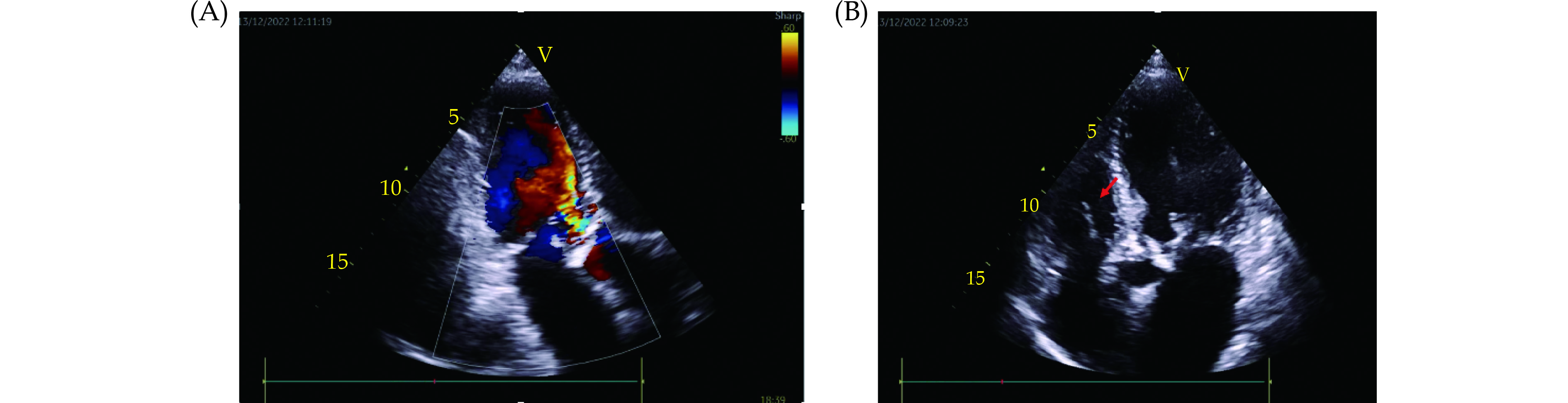
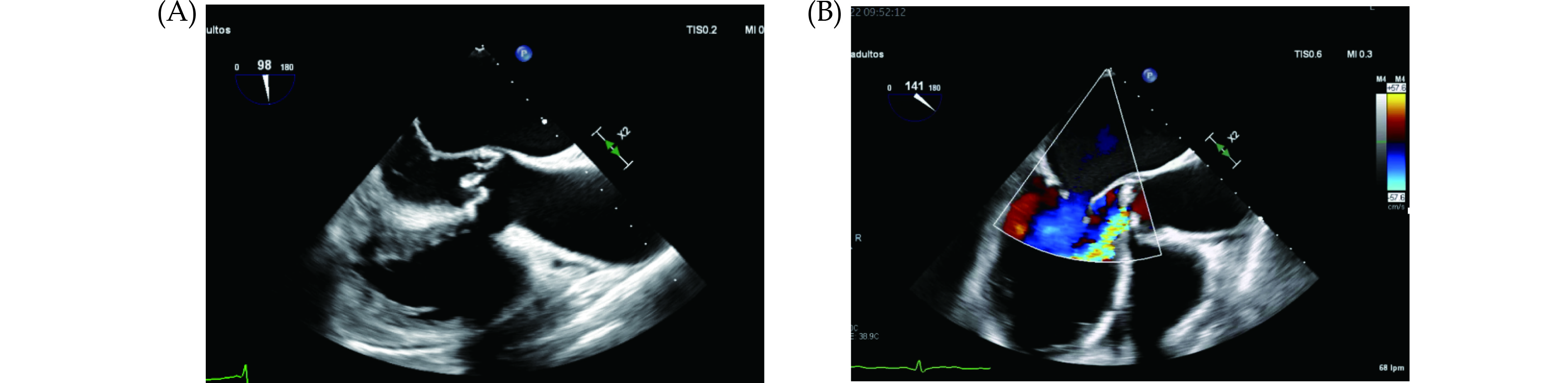
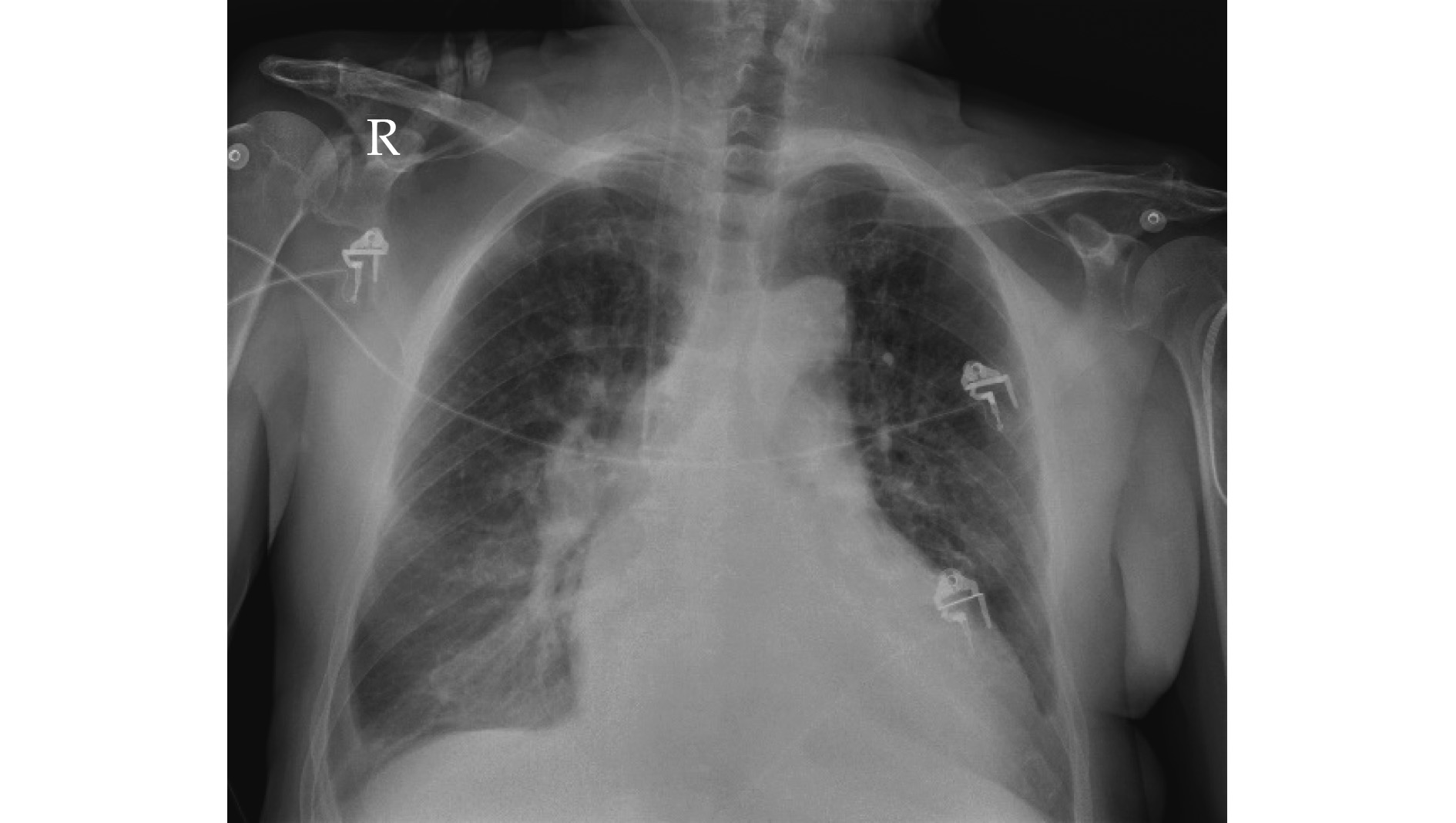
We present the case of an 88-year-old robust male with hypertension and permanent atrial fibrillation was admitted to our center with dyspnea and fever in the last month. On admission, he was tachypneic, with an oxygen saturation of 90%, blood pressure of 140/90 mmHg, a heart rate of 140 beats/min, and a chest X-ray with signs of acute pulmonary edema (Figure 1). Transthoracic echocardiography demonstrated vegetations on the tricuspid and aortic valves, with severe aortic regurgitation (Figure 2, Videos 1 and 2). The patient was treated with non-invasive ventilation, high-dose intravenous furosemide, and empirical antibiotic therapy (ceftriaxone, vancomycin, and gentamicin). Blood cultures were positive for Streptococcus agalactiae, sensitive to ceftriaxone, prompting adjustment of the antibiotic regimen. Transesophageal echocardiography confirmed infective endocarditis with severe aortic regurgitation (Figure 3, Videos 3 and 4). Despite initial management, the patient developed cardiogenic shock with hypotension requiring noradrenaline infusion, an increase in lactate levels to 2 mmol/L, and worsening of a previous normal renal function (creatinine 1.6 mg/dL). The case was discussed in the Heart Team multidisciplinary meeting, and due to the patient’s refusal of surgery and his high surgical risk, the decision was made to perform TAVI after confirming its feasibility with computer tomography scan. TAVI was successfully performed on day 8 of hospitalization, with the implantation of a balloon expandable valve through the right femoral artery. The procedure was uncomplicated, with only mild residual aortic regurgitation and no conduction disturbances (Figure 4, Video 5). The patient showed rapid hemodynamic improvement, allowing discontinuation of vasopressors and discharge two days post-procedure. At the two-year follow-up, the patient remains stable. He underwent node ablation and pacemaker implantation for rate control of atrial fibrillation. Echocardiography reveals only mild residual TAVI regurgitation, with no signs of recurrent endocarditis (Video 6).
TAVI has historically been sparingly used in cases of endocarditis. In fact, current guidelines do not recommended TAVI in aortic regurgitation and active infective endocarditis is considered a formal contraindication, as post-TAVI infective endocarditis is a dreaded complication.[5,7] However, a recent report suggests that the procedure can be performed safely and effectively in patients with residual aortic valve lesion but healed infection, with a one-year mortality rate comparable to those without infective endocarditis.[8] In addition, recent case reports have shown the feasibility of TAVI in active infective endocarditis.[3] Our case report is particularly remarkable as TAVI was done only 6 days after hospital admission, although blood cultures were negative at the time of implant. Given the high risks associated with surgical valve replacement in advanced aged patients with IE, TAVI may offer a less invasive alternative with favorable outcomes when carefully selected criteria are met, including negative blood cultures and absence of intracardiac complications (abscess, fistulas).
| [1] |
Perez-Rivera JA, Armiñanzas C, Muñoz P, et al. Comorbidity and Prognosis in Octogenarians with Infective Endocarditis. J Clin Med 2022; 11: 3774. doi: 10.3390/jcm11133774
|
| [2] |
Oliver L, Lavoute C, Giorgi R, et al. Infective endocarditis in octogenarians. Heart 2017; 103: 1602−1609.
|
| [3] |
Brankovic M, Hashemi A, Ansari J, et al. Transcatheter aortic valve replacement for aortic valve infective endocarditis: a systematic review and call for action. Cardiol Ther 2023; 12: 297.
|
| [4] |
Armiñanzas C, Fariñas-Alvarez C, Zarauza J, et al. Role of age and comorbidities in mortality of patients with infective endocarditis. Eur J Intern Med 2019; 64: 63−71.
|
| [5] |
Delgado V, Ajmone Marsan N, de Waha S, et al. 2023 ESC guidelines for the management of endocarditis. Eur Heart J 2023; 44: 3948−4042. doi: 10.1093/eurheartj/ehad193
|
| [6] |
Rawasia WF, Khan MS, Usman MS, et al. Safety and efficacy of transcatheter aortic valve replacement for native aortic valve regurgitation: a systematic review and meta-analysis. Catheter Cardiovasc Interv 2019; 93: 345−353.
|
| [7] |
del Val D, Panagides V, Mestres CA, et al. Infective endocarditis after transcatheter aortic valve replacement: JACC state-of-the-art review. J Am Coll Cardiol 2023; 81: 394−412.
|
| [8] |
Santos-Martínez S, Alkhodair A, Nombela-Franco L, et al. Transcatheter aortic valve replacement for residual lesion of the aortic valve following “healed” infective endocarditis. JACC Cardiovasc Interv 2020; 13: 1983−1996. doi: 10.1016/j.jcin.2020.05.033
|