| Citation: | Please cite this article as: HU SS. Rehabilitation of Cardiovascular Diseases in China. J Geriatr Cardiol 2024; 21(11): E1003−E1014. DOI: 10.26599/1671-5411.2024.11.007. |
The Annual Report on Cardiovascular Health and Diseases in China (2022) intricate landscape of cardiovascular health in China. In connection with the previous section, this 12th section of the report offers a comprehensive analysis of rehabilitation of cardiovascular diseases. In recent years, China’s cardiac rehabilitation has developed vigorously, and its clinical benefits have been proven by more and more evidences. More cardiac rehabilitation centers are built and standards are constantly being promoted. Despite the rapid development and progress, there are still major shortcomings in the current situation, such as lack of awareness among patients and families about the significance and importance of cardiac rehabilitation, and under participation in cardiac rehabilitation; the development of cardiac rehabilitation is uneven, with the majority concentrated in tertiary hospitals in economically developed areas; lack of high-level evidence-based evidences, quality control and safety standards need to be improved; the medical payment system is not thorough; lack of a systematic training and admission system, hindering the development of cardiac rehabilitation in China. Therefore, continuous efforts are needed to strengthen the construction of cardiac rehabilitation centers, which should sink from tertiary hospitals to secondary and primary medical service centers; encourage clinical research on cardiac rehabilitation; introduce consensus on quality control and safety standards; explore more on phase III cardiac rehabilitation; increase investment in integrating high-tech, artificial intelligence, etc. With the unique advantages of traditional Chinese medicine, exploring a Chinese characteristic cardiac rehabilitation model that is in line with China’s national conditions. Evidence-based medicine has confirmed that rehabilitation is the most effective method to reduce the disability rate of stroke, and it is also an indispensable key sector in the organized management model of stroke. Rehabilitation should span the entire process of stroke treatment. Perfecting the rehabilitation medical management system, steadily improving the rehabilitation medical service capacity, expanding diversified service methods, and emphasizing early and whole-range rehabilitation treatment have important clinical value and social significance for stroke rehabilitation.
Since the concept of cardiac rehabilitation was introduced into China in the 1980s, after nearly 40 years of exploration and practice, China’s cardiac rehabilitation work has been continuously advancing and has gained remarkable achievements.
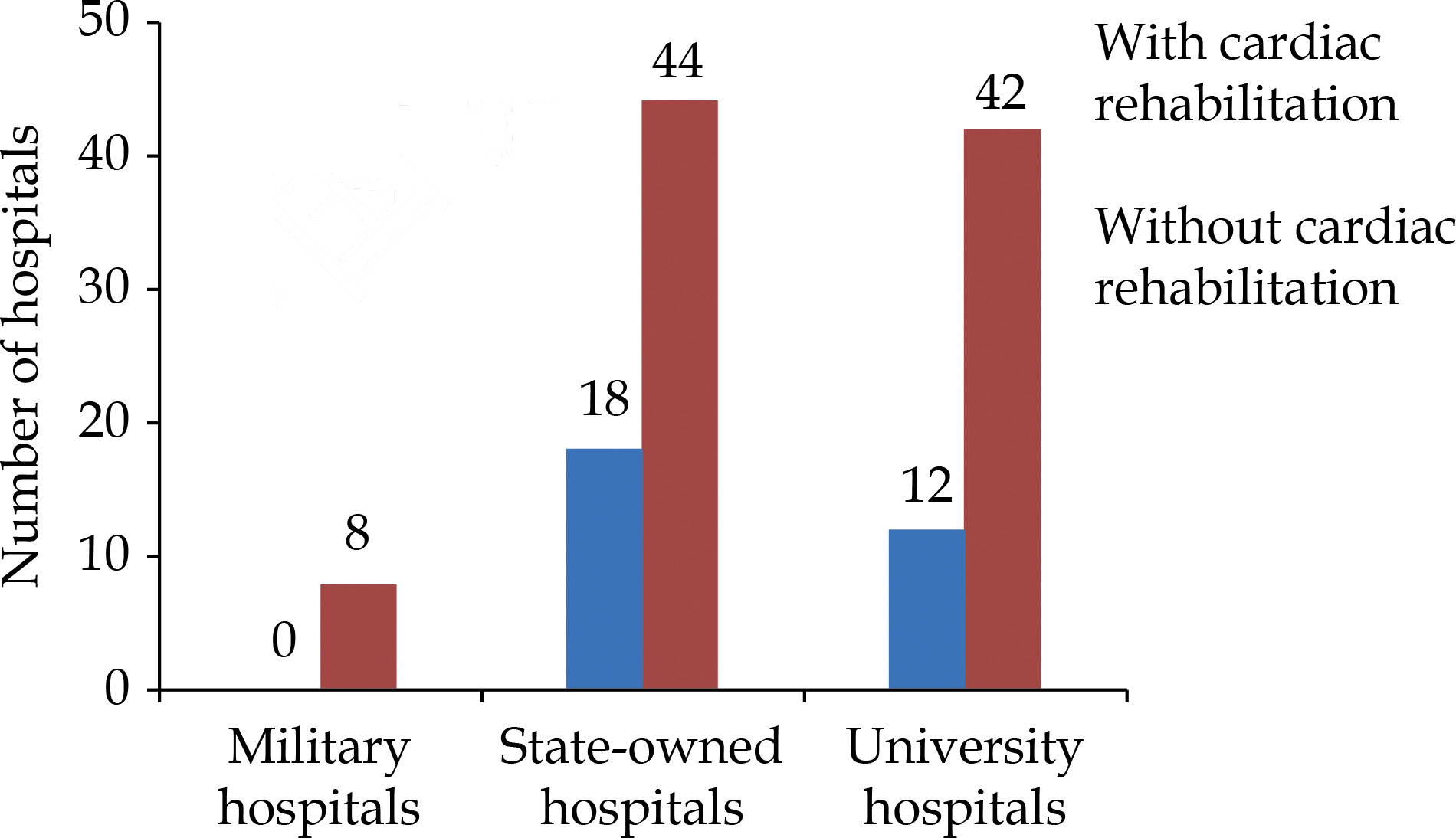
In 2016, a cross-sectional survey on the current status of cardiac rehabilitation in Chinese hospitals included 124 tertiary hospitals in 7 geographical regions of China.[1] The results showed that only 30 hospitals (24%) practiced cardiac rehabilitation, including 0 military hospital, 18 state-owned hospitals (29% of all surveyed state-owned hospitals), 12 university affiliated hospitals (22% of all surveyed university affiliated hospitals). It is revealed that cardiac rehabilitation work is mainly carried out in state-owned hospitals and university affiliated hospitals (Figure 1).
The result of the survey on the current status of cardiac rehabilitation in Chinese hospitals in 2016 showed that only 2.2 hospitals per 100 million population could carry out cardiac rehabilitation.[1] In terms of the distribution density in 7 geographical regions (number of cardiac rehabilitation centers/100 million population), developed regions such as North China, East China and South China are the most distributed, followed by the Northeast, Central and Southwest, while the Northwest has none, indicating that the development of cardiac rehabilitation in China is extremely uneven (Table 1).
| Region | Numbers of people/million | Numbers of cardiac rehabilitation centers | Density of cardiac rehabilitation centers/ (number/100 million population) |
| Northeast | 108 | 1 | 0.9 |
| North | 155 | 9 | 5.8 |
| East | 382 | 13 | 3.4 |
| Central | 240 | 2 | 0.8 |
| South | 147 | 4 | 2.7 |
| Southwest | 213 | 1 | 0.5 |
| Northwest | 99 | 0 | 0 |
| Total | 1,344 | 30 | 2.2 |
Cardiac rehabilitation (CR) is divided into three phases: phaseⅠ(inpatient CR), phaseⅡ (early outpatient CR) and phase Ⅲ (long-term outpatient CR). According to the survey on the current status of cardiac rehabilitation in Chinese hospitals in 2016, among the 13 hospitals that finished the complete 36-item survey and reported having a CR program, 3 hospitals (23%) offered phaseⅠ rehabilitation, 3 hospitals (23%) offered phaseⅡ rehabilitation, and 7 (54%) offered phaseⅠ+Ⅱ rehabilitation (Figure 2).[1]
(1) Effect of Chinese traditional Taijiquan exercise on prognosis of patients with coronary artery disease (CAD) after percutaneous coronary intervention (PCI)
A study investigated the effect of Taijiquan on the prognosis of patients with CAD after PCI.[2] 326 patients with CAD aged 57–71 years from March 2014 to March 2016 were randomly divided into control group and Tai Chi group. The control group was only given routine treatment, and the Tai Chi group was added with 24-style Yang Taijiquan besides routine treatment. The results of 6-month intervention showed that the scores of Exercise of Self-care Agency Scale (ESCA), Activities of Daily Living (ADL), SF-36 Questionnaire and left ventricular ejection fraction (LVEF) in the Tai Chi group were higher than those in the control group (P < 0.05). The arrhythmia incidence, recovery time of atrioventricular block, hospital stay and the scores of Self-rating Anxiety Scale (SAS) and Self-rating Depression Scale (SDS) were lower than those in the control group (P < 0.05). It is suggested that Taijiquan exercise could improve the prognosis of CAD patients after PCI (Table 2).
| Indicator | Taijiquan group (n = 128) | Control group (n = 121) | P-value |
| ESCA score | 122.5 ± 13.4 | 105.4 ± 12.5 | 0 |
| ADL score | 45.7 ± 6.5 | 39.6 ± 4.8 | 0.007 |
| SF-36 score | 61.5 ± 7.4 | 40.0 ± 5.3 | 0.001 |
| LVEF | 47.3% ± 3.4% | 42.6% ± 3.1% | 0.043 |
| Arrhythmia recovery time, day | 4.5 ± 1.2 | 6.3 ± 1.3 | 0.015 |
| Recovery time of atrioventricular block, day | 3.3 ± 1.6 | 5.5 ± 1.4 | 0.006 |
| Hospital stay, day | 16.4 ± 2.5 | 20.5 ± 4.8 | 0.032 |
| SAS/score | 32.3 ± 4.5 | 43.9 ± 5.6 | 0.001 |
| SDS/score | 39.2 ± 9.3 | 53.6 ± 8.7 | 0.003 |
| Data are presented as mean ± SD. LVEF: left ventricular ejection fraction; SAS: self-rating anxiety scale; SDS: self-rating depression scale. | |||
(2) Effect of Chinese traditional Baduanjin exercise on left ventricular (LV) remodeling and cardiac function in patients after acute myocardial infarction (AMI)
A randomized controlled study enrolled 110 clinically stable ST-segment elevation myocardial infarction (STEMI) patients who received coronary intervention treatment from January 2015 to October 2017, of whom 56 received 12 weeks of Baduanjin exercise cardiac rehabilitation (BE group), and the remaining 54 received 12 weeks of general exercise rehabilitation (control group).[3] The results showed that compared with the control group, the BE group showed significantly lower left ventricular end-diastolic volume index (ΔLVEDVi) (change from baseline to 6 months in the echocardiographic LV end-diastolic volume index) (–5.1 ± 1.1 vs. 0.3 ± 1.2 mL/m2, P < 0.01), and there was a greater increase in left ventricular ejection fraction (ΔLVEF) (4.2% ± 1.5% vs. 0.1% ± 1.2%, P < 0.05), suggesting that Baduanjin exercise (BE) could attenuate the adverse left ventricular (LV) remodeling, reduce ventricular dilation and improve ejection function in STEMI patients (Figure 3).
The safety of cardiac rehabilitation is the focus of attention. A prospective cohort study on the safety and efficacy of home-based cardiac rehabilitation included 335 patients with CAD after PCI from July 2015 to March 2018, they were divided into control group and home-based rehabilitation group.[4] Among them, the home-based rehabilitation group were remotely monitored through smartphones and corresponding software, and the longest follow-up was 42 months. Through propensity matching analysis, it was found that the incidence of major adverse cardiovascular event (MACE) in the home-based rehabilitation group was lower than that in the control group, and rehospitalization due to deteriorated angina pectoris was significantly decreased. The exercise ability, quality of life and control of CAD risk factors were better than those in the control group, which proved that the smartphone assisted home-based cardiac rehabilitation model was a safe and effective method to reduce cardiovascular risk and improve the health of patients with CAD (Table 3).
| Indicators | Control group (n = 135) | Home-based rehabilitation group (n = 135) |
P -value |
| MACE | 12 (8.9%) | 2 ( 1.5%) | 0.002 |
| AMI incidence | 0 | 0 | - |
| Unplanned revascularization | 12 (8.9%) | 2 ( 1.5%) | 0.002 |
| Stroke | 0 | 0 | |
| Cardiac death | 1 (0.6%) | 0 | 0.493 |
| Rehospitalization due to deteriorated angina pectoris | 31 (23%) | 13 (9.7%) | 0.002 |
| Max MET | 5.1 ± 1.4 | 6.2 ± 1.3 | 0.001 |
| VO2peak at anaerobic threshold, mL/kg per minute | 13.7 ± 4.1 | 16.2 ± 4.3 | < 0.001 |
| Systolic pressure, mmHg | 130.1 ± 13.9 | 122.2 ± 13.7 | < 0.001 |
| LDL-C, mmol/L | 2.2 ± 0.8 | 1.5 ± 0.6 | < 0.001 |
| Data are presented as mean ± SD or n (%). CAD: coronary artery disease; LDL-C: low-density lipoprotein cholesterol; MACE: major adverse cardiovascular event. | |||
Cardiac rehabilitation in China is gradually extending from center-based to home-based. However, as a novel thing, home-based cardiac rehabilitation is facing challenges. How to monitor to ensure safety and how to set, adjust and intervene are urgent problems to be solved.
A single-center, prospective, assessment-blinded, randomized controlled study included a total of 100 patients with atrial fibrillation after radiofrequency catheter ablation from February 2019 to July 2019.[5] They were randomized to a 12-week standard rehabilitation group (control group) or a comprehensive, domiciliary, mobile application-guided and telemonitored cardiac rehabilitation group (intervention group). Ninety seven patients completed follow-up. The results showed that the increase in VO2peak, the beliefs related to CVD and exercise self-efficacy scores in the intervention group was significantly higher than in the control group. It is suggested that remote home-based cardiac rehabilitation is necessary for atrial fibrillation patients after radiofrequency catheter ablation, and provides a promising alternative to conventional cardiac rehabilitation models (Table 4).
| Outcomes | Control group ( n = 48) | Intervention group ( n = 49) | P -value |
| VO2peak, mL/kg per minute | 4.9 ± 6.6 | 9.3 ± 8.0 | 0.003 |
| Beliefs related to CVD | 2.5 ± 15.2 | 11.1 ± 10.5 | 0.002 |
| Exercise self-efficacy | 4.2 ± 5.3 | 8.3 ± 4.8 | < 0.001 |
| CVD: cardiovascular diseases. | |||
Another prospective randomized controlled study included 96 patients with stable CAD, divided into control group and telemonitored group. Among them, the telemonitored group carried out remote monitoring through smartphones and corresponding software. After 6 months of follow-up, it was found that the cardiopulmonary and physical parameters and indexes and patients’ adherence in the telemonitored group were better than in the control group, which proved that the telemonitored cardiac rehabilitation model was effective for Chinese patients with CAD.[6]
A single-center prospective controlled study included 534 patients with MINOCA from August 2014 to October 2016 and randomized into a control group (CR-) and a cardiac rehabilitation group (CR+) to observe the impact of exercise-based cardiac rehabilitation on all-cause mortality and MACE in MINOCA patients.[7] The 3-year follow-up survival curve showed that compared with the CR-group, the all-cause mortality (log-rank P < 0.05) and MACE (log-rank P < 0.01) in the CR+ group were significantly reduced. It is suggested that exercise-based cardiac rehabilitation could significantly improve the prognosis of MINOCA patients (Figure 4).
A study, from January 2016 to January 2018, investigated the effect of early rehabilitation exercise on the prognosis of patients after cardiac surgery.[8] Eight hundred and ninety three patients after cardiac surgery and stayed in the ICU for more than 48 h were included. They were grouped in early rehabilitation group (239 patients) and conventional treatment group (654 patients) according to whether or not early rehabilitation was carried out. One hundred and ninety two cases from each group were matched by 1: 1 propensity score. The results showed that the mechanical ventilation duration was significantly shortened, the sedative drug use was reduced, the incidences of delirium and intestinal dysfunction were decreased, and the risk of malnutrition was reduced in the early rehabilitation group as compared to the conventional treatment group, suggesting that prognosis could be improved with early rehabilitation exercise after cardiac surgery (Table 5).
| Indicator | Early rehabilitation group (n = 192) | Conventional treatment group (n = 192) | P -value |
| Mechanical ventilation duration, h | 36.0 ± 14.9 | 43.0 ± 12.5 | 0.016 |
| Duration of sedative use, h | 39.0 ± 16.8 | 47.0 ± 21.3 | 0.001 |
| Delirium | 15 (7.81%) | 33 (17.19%) | 0.006 |
| Intestinal dysfunction | 51 (26.56%) | 82 (42.71%) | 0.001 |
| Triceps skinfold thickness, mm | 15.0 ± 2.8 | 12.0 ± 3.3 | 0.021 |
| Data are presented as mean ± SD or n (%). | |||
A single-center, randomized controlled study analyzed the impact of precision implementation of early ambulation on the prognosis of elderly patients undergoing off-pump coronary artery bypass grafting (CABG).[9] A total of 178 patients aged ≥ 60 years who underwent off-pump CABG were enrolled in this study. The patients were randomized to either the precision implementation of early ambulation group (PEA group) or the conventional ambulation group (control group). A precision early ambulation plan, based on the age projected maximum heart rate and maximum oxygen uptake (VO2max), was developed for the PEA group. The results showed that in the intention-to-treat analysis, the postoperative hospital stay of the PEA group (9.04 ± 3.08 days) was significantly shorter than that of the control group (10.09 ± 3.32 days).
A study of evaluation on the effect of early comprehensive rehabilitation in children with congenital heart disease after surgery analyzed length of hospital stay, hospitalization cost of 400 children with congenital heart disease (aged between 6 months and 3 years old) undergoing heart surgery from January 2007 to December 2018.[10] The patients were randomly divided into rehabilitation group and control group. The rehabilitation group was given comprehensive rehabilitation intervention measures, and the control group was given conventional intervention measures. The results showed that the length of hospital stay of rehabilitation group was obviously shortened (P < 0.001) and hospitalization cost lowered (P < 0.001), suggesting that comprehensive rehabilitation could significantly reduce the hospitalization time and cost of children with congenital heart disease (Table 6).
| Group | Hospitalization time/d | Hospitalization cost/CNY |
| Rehabilitation group (n = 200) | 4.2 ± 2.1 | 38,132 ± 9,502 |
| Control group (n = 200) | 6.6 ± 3.2 | 42,867 ± 13,516 |
| P-value | < 0.001 | < 0.001 |
| Data are presented as mean ± SD. | ||
In recent years, cardiac rehabilitation has developed rapidly in China, and relevant institutes have issued rehabilitation guidelines successively (Table 7). These programmatic documents systematically elaborated the definition and benefit evidence of cardiac rehabilitation, clarified the standardized process, risk control and quality control measures, and formulated the basic norms for the construction of cardiac rehabilitation departments.
| Release time | Name |
| 2018 | China cardiac rehabilitation and secondary prevention guideline 2018 Essentials[11] |
| 2018 | Chinese expert consensus on exercise rehabilitation of patients with stable CAD aged 75 and above[12] |
| 2020 | Expert consensus on cardiac rehabilitation after CABG[13] |
| 2020 | Chinese expert consensus on cardiac rehabilitation of chronic heart failure[14] |
| 2021 | Chinese expert consensus on cardiac rehabilitation of patients with atrial fibrillation[15] |
| 2021 | Chinese expert consensus on exercise rehabilitation for adult patients with pulmonary hypertension[16] |
| 2022 | Chinese expert consensus on the clinical normative application of 6MWT[17] |
| 2022 | Chinese expert consensus on home-based rehabilitation for patients with cardiovascular diseases[18] |
| CABG: coronary artery bypass grafting; CAD: coronary artery disease. | |
The number of rehabilitation beds in Chinese medical institutions continues to increase (Figure 5), and it was 246,907 nationwide in 2020, and the top five provinces in terms of bed numbers were Jiangsu, Zhejiang, Henan, Shandong, and Guangdong (Figure 6).[19] The number of rehabilitation practitioners is also constantly increasing. A national survey in 2009 found that there were 16,000 physicians, 14,000 therapists, and 12,000 nurses engaging in medical rehabilitation. In 2018, the number of rehabilitation physicians and nurses in China increased to 38,000 and 15,000 respectively.[20]
In recent years, Chengdu, Shenzhen, Shanghai, Jiangsu and Hebei conducted surveys on the bed and personnel structure of rehabilitation departments using survey questionnaires or online questionnaires.
In 2018, the Chengdu Rehabilitation Quality Control Center conducted a questionnaire survey on the number of beds and staffing in comprehensive hospitals, rehabilitation medical departments of traditional Chinese medicine hospitals, and rehabilitation hospitals in 22 districts (cities) and counties of Chengdu. The survey results showed that there were a total of 514 rehabilitation physicians and 415 therapists in rehabilitation departments of 66 secondary or above medical institutions, among which, 43 medical institutions had inpatient service in their rehabilitation departments, with a total of 1,781 designated beds. In 2019, the Chengdu Rehabilitation Quality Control Center conducted on-site investigation on 37 designated rehabilitation medical insurance institutions within the jurisdiction of Chengdu, including 1 National Health Commission affiliated medical institution, 7 provincial medical institutions, and 29 municipal medical institutions. The survey showed that there were a total of 681 rehabilitation physicians and 716 rehabilitation therapists in these institutions.[21]
From September to November 2019, Shenzhen conducted an online survey of 55 medical institutions with rehabilitation departments, and there were a total of 3,312 beds, 629 rehabilitation physicians, 902 therapists, and 790 nurses.[22]
From June to July 2020, Shanghai conducted a survey of 311 tertiary, secondary, primary, and unranked medical institutions. Among them, 254 medical institutions had rehabilitation departments, with a total of 1,414 rehabilitation physicians, 2,668 rehabilitation therapists, and 1,614 rehabilitation nurses.[23]
From December 2019 to October 2020, researchers in Jiangsu surveyed a total of 666 primary medical institutions through the “National Rehabilitation Medical Resource Survey System” network platform, with a total of 395 (59.31%) having rehabilitation departments or general practice clinics mainly focused on rehabilitation. Among them, 223 hospitals provided inpatient service, with a total of 3,967 beds of rehabilitation as the main function. There were a total of 234 rehabilitation physicians, 725 rehabilitation therapists, and 2,047 nurses in these 395 primary medical institutions.[24]
From November to December 2020, staff in Hebei distributed WeChat questionnaires to 132 county-level comprehensive hospitals in the province, of which 107 hospitals had rehabilitation departments and had a total of 1,805 designated beds.[25]
From August 2015 to July 2019, a multi-center study involving 1,312 hospitals investigated factors related to rehabilitation assessment in hospitalized patients with cerebral hemorrhage and the relationship between rehabilitation assessment and prognosis during hospitalization. A total of 85,664 intracerebral hemorrhage patients were included, with an average age of 62.9 ± 12.9 years, and 37.5% were female. The results showed that 62,228 (72.6%) patients were assessed for rehabilitation. In multivariate analysis, patients with a history of hypertension, a history of peripheral artery disease, a higher Glasgow Coma Scale score at admission, dysphagia screening, carotid vessel imaging, and a longer length of hospital stay were more likely to undergo rehabilitation assessments. On the contrary, patients admitted to intensive care units and tertiary hospitals were less likely to be assessed during hospitalization. Urban residents with basic medical insurance were more likely to receive assessment than self-funded patients. Compared to patients who did not get rehabilitation assessment, those got rehabilitation assessment had longer hospital stays and lower in-hospital mortality.[26]
Early rehabilitation could help improve the neurological functions of patients with acute ischemic or hemorrhagic stroke, reduce the incidence of deep vein thrombosis, and improve their quality of life, but the time point for early or ultra early rehabilitation is still controversial.[27]
A study divided 86 patients with ischemic stroke into an ultra early rehabilitation group of 41 cases (within 72 hours of onset) and an early rehabilitation group of 45 cases (within 72 h to 7 days of onset). Except for different intervention time points, the rehabilitation plans of the two groups were the same. The results showed that the National Institutes of Health Stroke Scale (NIHSS) and Fugl-Meyer Assessment (FMA) scores of patients in the ultra early rehabilitation group were significantly higher than those in the early rehabilitation group at 1 month and 3 months of onset, and the rehabilitation efficacy of the ultra early group was better than that of the early group.[28] Another study compared the difference between patients starting rehabilitation treatment 24 to 48 h after onset (early rehabilitation group) and 72 to 96 hours after onset (standard rehabilitation group). One hundred and ten patients were randomized into two groups and received physical rehabilitation therapy including limb movement, stretching, rolling, bed sitting, standing, physical strength, and daily living ability training on the affected side. The results showed that compared to the standard rehabilitation group, the early rehabilitation group showed a decrease in the modified Rankin Scale (mRS) score at 90 days of onset, and a significant improvement in the lower extremity FMA score in the first week after stroke onset. However, there was no significant difference in the lower extremity motor function scores between the two groups at 3 months.[29]
A study on early rehabilitation training of patients with hemorrhagic stroke included a total of 82 patients, with 41 in the early intervention group and 41 in the control group. The study found that compared to rehabilitation training within 3 to 4 weeks after onset, early intervention training between 2 and 7 days after onset was more beneficialfor improving motor function, neurological function, and daily living abilities in patients with hemorrhagic stroke.[30]
There is a lack of evidence for the benefits of early rehabilitation in patients with acute ischemic stroke after endovascular treatment. A multi-center, prospective study evaluated early rehabilitation on outcomes in stroke patients with large vessel occlusion who received endovascular treatment. 1,126 patients were divided into the early rehabilitation group [273 patients (24.2%) starting rehabilitation within one week of onset] and the standard care group of 853 patients (75.8%). The early rehabilitation group received rehabilitation intervention for 45 min per day, 5–7 days per week, on the basis of standard care treatment, with a maximum intervention time of 14 days. Although there was no significant difference in functional recovery (mRS 0-2) between the two groups at 90 days of onset, compared to the standard care group, early rehabilitation group had a lower 90-day mortality (6.2% vs. 20.5%, P < 0.01).[31]
Traditional Chinese medicine and health preservation methods (such as Qigong, Baduanjin, acupuncture and, etc.) combined with modern medical technology are increasingly used in the rehabilitation of stroke patients. Liuzijue Qigong combining conventional phonetic training could effectively improve the respiratory function and speech ability of patients with post-stroke motor aphasia.[32] Combining conventional breathing training could improve trunk control ability, respiratory muscle function, and daily living activity ability in early stroke patients.[33] Combining basic vocal training could improve the respiratory control ability and comprehensive speech ability of stroke patients with dysarthria.[34] Combining conventional rehabilitation training could improve the balance function of stroke patients.[35] Baduanjin exercise could ameliorate limb motor function, balance function, muscle strength, and gait in patients with post-stroke cognitive impairment.[36] Interactive dynamic scalp acupuncture combined with lower limb robot training could effectively enhance the lower extremity motor function and walking ability of stroke patients.[37]
The application of new technologies in the rehabilitation of stroke patients has also achieved some results. Brain-computer interface-operated lower limb rehabilitation robot and Sensorimotor rhythm-brain computer interface could improve the motor function of stroke patients and promote the recovery of cognitive function.[38–40] Immersive virtual reality environment could improve the upper extremity function of stroke patients, and transcutaneous auricular vagal nerve stimulation combined with conventional rehabilitation training could significantly improve the motor and sensory functions of stroke patients.[41,42] An exoneuromusculoskeleton driven by electromyography could improve upper limb muscle coordination.[43]
The International Classification of Functioning, Disability and Health (ICF) Core Set for Stroke could be used to evaluate the function, structure, activity and participation, and environmental factors of stroke rehabilitation patients. Research under the ICF framework could improve lower extremity motility, speech function, and evaluate swallowing function. Based on ICF Core Set, 113 stroke patients were selected and divided into the ischemic group (n = 67) and the hemorrhagic group (n = 46). Lower extremity exercise included joint function training, muscle strength training, endurance training, walking training, and wheelchair training. Patients were equipped with foot pads to provide plantar sound feedback. Both groups received lower limb motor training with plantar sound feedback, with a duration of 30 min per session, twice a day, for a total of 8 weeks. The gait part of the ICF Core Set for Stroke, the lower extremity part of the Fugl-Meyer Assessment (FMA-LE), the timed “up & go” test (TUGT), and the modified Barthel Index (MBI) were used for evaluation. The results showed that the combination of exercise therapy and plantar sound feedback could significantly improve the lower extremity motility, movement, and daily living activities of hemiplegic gait patients after stroke.[44] A study used the “Speech Cognitive Assessment Training and Interaction” software under the ICF framework to train stroke patients with naming disorders, including naming training, continuation training, and listing training. The control group was given conventional speech training including naming images and objects, listening and retelling stimuli, and eliciting objects or images. Both groups trained for 40 minutes per session, 5 sessions per week, for a total of 1 month. The naming part of the Western Aphasia Batter was used for effectiveness evaluation. After 2 and 4 weeks of treatment, the software training group’s naming score significantly increased, indicating that the naming disorder rehabilitation of the “Speech Cognitive Assessment Training and Interaction” aphasia training system under the ICF framework could effectively improve the naming disorder of stroke patients.[45]
A study on the correlation between ICF-d560 and swallowing function in convalescent stroke patients included 140 convalescent stroke patients with swallowing disorders hospitalized in the rehabilitation department. The subjects were evaluated by two rehabilitation physicians trained through ICF clinical practice. According to ICF-d560, dysphagia was classified into 1–4 levels (1–10 points), and according to the modified Kubota Water Swallowing Test, dysphagia was classified as mild, moderate, and severe. The impact of various clinical risk factors on the screening results of dysphagia was analyzed with the Enter method in linear regression, and the correlation between ICF-d560 and the modified Kubota Water Swallowing Test was explored with Spearman correlation analysis. The results indicated that ICF-d560 had a good correlation with the modified Kubota Water Swallowing Test and could be used as a swallowing function screening tool under the ICF framework.[46]
With the advances of the three-level rehabilitation and Internet technology, a community-family-smart technology assisted rehabilitation model, suitable for the current national conditions, is being explored for stroke rehabilitation. Remote rehabilitation can deliver rehabilitation services through information and communication technology to make up for the current shortage of stroke rehabilitation resources, especially during the pandemic period.
A 6-month study conducted at 3 community health service centers in Fengtai District, Beijing, found that receiving remote rehabilitation guidance from home during community outpatient rehabilitation could improve rehabilitation outcomes for stroke patients. This study randomly divided 240 stroke recovery patients into a control group and a remote rehabilitation group of 120 each. Both groups received community rehabilitation outpatient treatment for 6 months, no less than 3 times a week, and no less than 1 h each time. The remote rehabilitation group received remote rehabilitation guidance through online communication platforms, 2–3 times a week, for about 30 min each time. The results showed that the BI and FMA scores of the remote group were higher than those of the control group.[47] A study on task oriented training for discharged stroke patients through remote rehabilitation platforms showed that task oriented training implemented through remote rehabilitation platforms could improve stroke patients’ motor function and activities of daily living (ADL). The study randomly divided 80 patients into a control group and a treatment group, with 40 patients in each group. The control group patients made outpatient follow-up visits once a week, and a task oriented training plan was developed by rehabilitation therapists. Patients were required to undergo systematic upper and lower extremity training at home or at the community health service center, twice a day for 60 min each time; The treatment group received follow-up visits through a remote rehabilitation platform, and the rehabilitation therapist developed task oriented training for the patients remotely. Under remote guidance, supervision, and real-time adjustment of the therapist, the patients did 60 min of upper and lower limb training twice a day. At 4 and 8 weeks of treatment, the BI and FMA scores of the remote group were higher than those of the control group.[48] A 12-week prospective randomized controlled study conducted by Zhongshan Hospital of Fudan University in Shanghai also showed that home-based telerehabilitation improved motor function in stroke patients, and was safe and feasible.[49]
A community-based rehabilitation for patients with cerebral hemorrhage showed that 3–6 months of community-based rehabilitation not only promoted the recovery of neurological functions, but also improved their medication compliance and quality of life.[50] The results of a randomized controlled study on the hospital-community integrated service model conducting on 120 elderly stroke patients after discharge showed that applying the hospital-community integrated service model to home rehabilitation of stroke in disabled elderly could improve their self-care ability and self-efficacy, improve medical compliance, and reduce negative emotions.[51]
A study of a transitional home-based care program after stroke randomly divided 116 patients with ischemic stroke into an intervention group (n = 58) and a control group (n = 58). The intervention group received a 12-week transitional home-based care program. This program was developed by a team of 1 physical therapist, 1 occupational therapist, 1 speech therapist, 1 neurologist, and 1 rehabilitation doctor based on national guidelines of China, the United States, and Canada. It included one pre-discharge meeting, six post-discharge home visits (odd weeks), and six telephone follow-up visits (even weeks), with a dedicated hotline managed by nurses available for communication throughout the entire 12 weeks. The control group received medication advice, rehabilitation training, and telephone follow-ups from nurses. Research found that this home-based transitional care program could improve stroke patients’ quality of life, ADL, and self-efficacy at 90 and 180 days of intervention.[52]
In January 2022, experts from the Neurorehabilitation Group of Chinese Society of Neurology, the Cerebrovascular Disease Professional Committee of the Chinese Association of Rehabilitation Medicine and the China Rehabilitation Research Center issued the Expert Consensus on Clinical Management of Post-stroke Aphasia, which provides evidence-based medical evidences for standardized clinical management and common clinical issues of post-stroke aphasia, and provides clinical guidance for the rehabilitation of post-stroke aphasia patients.[53]
| [1] |
Zhang Z, Pack Q, Squires RW, et al. Availability and characteristics of cardiac rehabilitation programmes in China. Heart Asia 2016; 8: 9−12. doi: 10.1136/heartasia-2016-010758
|
| [2] |
Li Y, Zhang HY, Wang YS. Tai Chi ameliorates coronary heart disease by affecting serum levels of miR-24 and miR-155. Front Physiol 2019; 10: 587. doi: 10.3389/fphys.2019.00587
|
| [3] |
Mao S, Zhang XX, Chen MG, et al. Beneficial effects of baduanjin exercise on left ventricular remodelling in patients after acute myocardial infarction: an exploratory clinical trial and proteomic analysis. Cardiovasc Drugs Ther 2021; 35: 21−32. doi: 10.1007/s10557-020-07047-0
|
| [4] |
Ma J, Ge C, Shi YJ, et al. Chinese home-based cardiac rehabilitation model delivered by smartphone interaction improves clinical outcomes in patients with coronary heart disease. Front Cardiovasc Med 2021; 8: 731557. doi: 10.3389/fcvm.2021.731557
|
| [5] |
Cai C, Bao ZP, Wu N, et al. A novel model of home-based, patient-tailored and mobile application-guided cardiac telerehabilitation in patients with atrial fibrillation: A randomised controlled trial. Clin Rehabil 2022; 36: 40−50. doi: 10.1177/02692155211032372
|
| [6] |
Song YX, Ren C, Liu P, et al. Effect of smartphone-based telemonitored exercise rehabilitation among patients with coronary heart disease. J Cardiovasc Transl Res 2020; 13: 659−667. doi: 10.1007/s12265-019-09938-6
|
| [7] |
He CJ, Zhu CY, Zhu YJ, et al. Effect of exercise-based cardiac rehabilitation on clinical outcomes in patients with myocardial infarction in the absence of obstructive coronary artery disease (MINOCA). Int J Cardiol 2020; 315: 9−14. doi: 10.1016/j.ijcard.2020.05.019
|
| [8] |
Wang SP, Meng SP, Chen HJ, et al. [Effects of early rehabilitation exercise on prognosis of patients after cardiac surgery]. Zhongguo Xunhuan Zazhi 2019; 34: 498–502. [Article in Chinese].
|
| [9] |
Cui ZM, Li N, Gao CN, et al. Precision implementation of early ambulation in elderly patients undergoing off-pump coronary artery bypass graft surgery: a randomized-controlled clinical trial. BMC Geriatr 2020; 20: 404. doi: 10.1186/s12877-020-01823-1
|
| [10] |
Liu Z, Chen XY, Chen DY, et al. [Evaluation of early comprehensive intervention rehabilitation mode after congenital heart disease surgery in children]. Lingnan Xinxueguan Bing Zazhi 2017; 23: 448–450, 478. [Article in Chinese].
|
| [11] |
Cardiovascular Disease Professional Committee of Chinese Association of Rehabilitation Medicine. [Chinese guidelines for cardiac rehabilitation and secondary prevention 2018]. Zhonghua Neike Zazhi 2018; 57: 802–810. [Article in Chinese].
|
| [12] |
Geriatrics Branch of Chinese Medical Association. [Chinese expert consensus on exercise rehabilitation for patients with stable coronary heart disease aged 75 and above]. Zhongguo Zonghe Linchuang 2018; 34: 97–104. [Article in Chinese].
|
| [13] |
National Center for Cardiovascular Diseases. [Expert consensus on cardiac rehabilitation after coronary artery bypass grafting]. Zhongguo Xunhuan Zazhi 2020; 35: 4–15. [Article in Chinese].
|
| [14] |
Cardiovascular Disease Prevention and Rehabilitation Professional Committee of Chinese Association of Rehabilitation Medicine. [Chinese expert consensus on cardiac rehabilitation for chronic heart failure]. Zhonghua Neike Zazhi 2020; 59: 942–952. [Article in Chinese].
|
| [15] |
Cardiovascular Disease Prevention and Rehabilitation Professional Committee of Chinese Association of Rehabilitation Medicine. [Chinese expert consensus on cardiac rehabilitation for patients with atrial fibrillation]. Zhonghua Neike Zazhi 2021; 60: 106–116. [Article in Chinese].
|
| [16] |
Cardiovascular Physician Branch of Chinese Medical Doctor Association, Cardiac Rehabilitation Management Professional Committee of Chinese Hospital Association. [Chinese expert consensus on exercise rehabilitation for adult patients with pulmonary hypertension]. Zhongguo Jieru Xinzangbing Xue Zazhi 2021; 29: 421–432. [Article in Chinese].
|
| [17] |
Cardiovascular Branch of Chinese Medical Association, Cardiopulmonary Prevention and Rehabilitation Professional Committee of Chinese Association of Rehabilitation Medicine, Editorial Committee of Chinese Journal of Cardiovascular Diseases. [Chinese expert consensus on clinical standardized application of six-minute walk test]. Zhonghua Xinxueguan Bing Zazhi 2022; 50: 432–442. [Article in Chinese].
|
| [18] |
[Chinese expert consensus on home rehabilitation for cardiovascular disease patients]. Zhongguo Xunhuan Zazhi 2022; 37: 108–121. [Article in Chinese].
|
| [19] |
National Health Commission of the People's Republic of China. China Health Statistics Yearbook 2021. Beijing: Peking Union Medical College Press, 2021.
|
| [20] |
Li JN, Li LSW. Development of rehabilitation in China. Phys Med Rehabil Clin N Am 2019; 30: 769−773. doi: 10.1016/j.pmr.2019.07.010
|
| [21] |
Luo L, Yuan JL, Li P, et al. [Current situation and thinking of rehabilitation medical personnel allocation in Chengdu]. Zhonghua Wuli Yixue Yu Kangfu Zazhi 2021; 43: 451–453. [Article in Chinese].
|
| [22] |
Gao Y, Wang YL, Chen WS, et al. [Investigation on the current situation of rehabilitation medical resource allocation in Shenzhen]. Zhongguo Kangfu Yixue Zazhi 2021; 36: 326–329. [Article in Chinese].
|
| [23] |
Zheng JJ, Shen LY, Duan LR, et al. [Current situation of rehabilitation human resources development in Shanghai]. Zhongguo Kangfu Lilun Yu Shijian 2020; 26: 1471–1476. [Article in Chinese].
|
| [24] |
Wang Y, Liu XR, Xu GX, et al. [Current situation and regional comparative analysis of grassroots rehabilitation medical resources in Jiangsu Province]. Zhongguo Kangfu Yixue Zazhi 2022; 37: 519–522. [Article in Chinese].
|
| [25] |
Zhang L, Sun ZX, Yan YN, et al. [Investigation on the current situation of rehabilitation medicine department and stroke rehabilitation treatment in county-level public general hospitals in Hebei Province]. Zhongguo Kangfu Yixue Zazhi 2022; 37: 789–792, 797. [Article in Chinese].
|
| [26] |
Sun JJ, Deng YM, Wang DD, et al. Assessment of rehabilitation following intracerebral hemorrhage in China: findings from the Chinese stroke center alliance. Neurol Res 2022; 20: 1−9.
|
| [27] |
Hu LJ, Liu GW. Effects of early rehabilitation nursing on neurological functions and quality of life of patients with ischemic stroke hemiplegia. Am J Transl Res 2021; 13: 3811−3818.
|
| [28] |
Liu LL, Lu YQ, Bi QQ, et al. Effects of different intervention time points of early rehabilitation on patients with acute ischemic stroke: A single-center, randomized control study. Biomed Res Int 2021; 2021: 1940549. doi: 10.1155/2021/1940549
|
| [29] |
Wang FD, Zhang S, Zhou FH, et al. Early physical rehabilitation therapy between 24 and 48 h following acute ischemic stroke onset: a randomized controlled trial. Disabil Rehabil 2022; 44: 3967−3972. doi: 10.1080/09638288.2021.1897168
|
| [30] |
Yu JJ, Zhou F, Zhang Y. Comparison of early interventional rehabilitation training with delayed training on motor function recovery in patients with cerebral haemorrhage. J Pak Med Assoc 2020; 70: 71−77.
|
| [31] |
He Y, Nie XM, He T, et al. Impact of early rehabilitation on outcomes in patients with acute ischemic stroke after endovascular treatment. Front Neurol 2022; 13: 877773. doi: 10.3389/fneur.2022.877773
|
| [32] |
Ding SS, Li GY, Wang J, et al. [Multicenter clinical study of "Six-Character Formula" training in the treatment of motor speech disorders after stroke]. Zhonghua Wuli Yixue Yu Kangfu Zazhi 2021; 43: 890–894. [Article in Chinese].
|
| [33] |
Zheng YN, Zhang Y, Li HL, et al. Comparative effect of liuzijue qigong and conventional respiratory training on trunk control ability and respiratory muscle function in patients at an early recovery stage from stroke: A randomized controlled trial. Arch Phys Med Rehabil 2021; 102: 423−430. doi: 10.1016/j.apmr.2020.07.007
|
| [34] |
Wang J, Li GY, Ding SS, et al. Liuzijue qigong versus traditional breathing training for patients with post-stroke dysarthria complicated by abnormal respiratory control: Results of a single-center randomized controlled trial. Clin Rehabil 2021; 35: 999−1010. doi: 10.1177/0269215521992473
|
| [35] |
Zhang Y, Wang C, Yang JZ, et al. Comparing the effects of short-term liuzijue exercise and core stability training on balance function in patients recovering from stroke: A pilot randomized controlled trial. Front Neurol 2022; 13: 748754. doi: 10.3389/fneur.2022.748754
|
| [36] |
Ye MZ, Zheng YH, Xiong ZY, et al. Baduanjin exercise ameliorates motor function in patients with post-stroke cognitive impairment: A randomized controlled trial. Complement Ther Clin Pract 2022; 46: 101506. doi: 10.1016/j.ctcp.2021.101506
|
| [37] |
Zhang SH, Wang YL, Zhang CX, et al. Effects of interactive dynamic scalp acupuncture on motor function and gait of lower limbs after stroke: A multicenter, randomized, controlled clinical trial. Chin J Integr Med 2022; 28: 483−491. doi: 10.1007/s11655-021-3525-0
|
| [38] |
Li C, Wei JY, Huang XQ, et al. Effects of a brain-computer interface-operated lower limb rehabilitation robot on motor function recovery in patients with stroke. J Healthc Eng 2021; 2021: 4710044.
|
| [39] |
Li X, Wang L, Miao S, et al. Sensorimotor rhythm-brain computer interface with audio-cue, motor observation and multisensory feedback for upper-limb stroke rehabilitation: A controlled study. Front Neurosci 2022; 16: 808830. doi: 10.3389/fnins.2022.808830
|
| [40] |
Zhao CG, Ju F, Sun W, et al. Effects of training with a brain-computer interface-controlled robot on rehabilitation outcome in patients with subacute stroke: A randomized controlled trial. Neurol Ther 2022; 11: 679−695. doi: 10.1007/s40120-022-00333-z
|
| [41] |
Mekbib DB, Debeli DK, Zhang L, et al. A novel fully immersive virtual reality environment for upper extremity rehabilitation in patients with stroke. Ann N Y Acad Sci 2021; 1493: 75−89. doi: 10.1111/nyas.14554
|
| [42] |
Li JN, Xie CC, Li CQ, et al. Efficacy and safety of transcutaneous auricular vagus nerve stimulation combined with conventional rehabilitation training in acute stroke patients: a randomized controlled trial conducted for 1 year involving 60 patients. Neural Regen Res 2022; 17: 1809−1813. doi: 10.4103/1673-5374.332155
|
| [43] |
Nam CY, Rong W, Li WM, et al. An exoneuromusculoskeleton for self-help upper limb rehabilitation after stroke. Soft Robot 2022; 9: 14−35. doi: 10.1089/soro.2020.0090
|
| [44] |
Cui WH, Wang ML, Yang QS, et al. [Study on rehabilitation effect of lower limb motor function after stroke based on ICF core classification combination exercise therapy combined with plantar sound induction method]. Zhongguo Kangfu Lilun Yu Shijian 2021; 27: 249–255. [Article in Chinese].
|
| [45] |
Wang XW, Tang RK, Qian H, et al. [Study on the effect of speech and language training on naming disorders in stroke patients under ICF framework]. Tingli Xue Yu Yuyan Jibing Zazhi 2021; 29: 499–503. [Article in Chinese].
|
| [46] |
Xu WW, Chen Y, Han Y, et al. [Correlation analysis between ICF-d560 and swallowing function in stroke patients during recovery period]. Zhonghua Wuli Yixue Yu Kangfu Zazhi 2021; 43: 607–610. [Article in Chinese].
|
| [47] |
Liu HL, Zhou B, Zhao Z, et al. [Observation on the effect of home remote rehabilitation guidance for stroke patients]. Zhongguo Kangfu Lilun Yu Shijian 2021; 27: 807–811. [Article in Chinese].
|
| [48] |
Wu HL, Zhang Y, Wang A, et al. [Effect of task-oriented training based on remote rehabilitation platform on motor function and activities of daily living ability in post-discharge stroke patients]. Zhonghua Wuli Yixue Yu Kangfu Zazhi 2022; 44: 40–43. [Article in Chinese].
|
| [49] |
Chen J, Sun DL, Zhang SF, et al. Effects of home-based telerehabilitation in patients with stroke: A randomized controlled trial. Neurology 2020; 95: e2318−e2330.
|
| [50] |
Qian H, Chen SX, Chen YR, et al. Community-based rehabilitation promotes the functional recovery of patients after intracerebral hemorrhage. Neurologist 2022; 27: 89−94. doi: 10.1097/NRL.0000000000000375
|
| [51] |
Feng WJ, Yu H, Wang J, et al. Application effect of the hospital-community integrated service model in home rehabilitation of stroke in disabled elderly: a randomised trial. Ann Palliat Med 2021; 10: 4670−4677. doi: 10.21037/apm-21-602
|
| [52] |
Wong FKY, Wang SL, Ng SSM, et al. Effects of a transitional home-based care program for stroke survivors in Harbin, China: a randomized controlled trial. Age Ageing 2022; 51: afac027. doi: 10.1093/ageing/afac027
|
| [53] |
Zhang T, Li SL, Bai YL, et al. [Expert consensus on clinical management of post-stroke aphasia]. Zhongguo Kangfu Lilun Yu Shijian 2022; 28: 15–23. [Article in Chinese].
|
| Region | Numbers of people/million | Numbers of cardiac rehabilitation centers | Density of cardiac rehabilitation centers/ (number/100 million population) |
| Northeast | 108 | 1 | 0.9 |
| North | 155 | 9 | 5.8 |
| East | 382 | 13 | 3.4 |
| Central | 240 | 2 | 0.8 |
| South | 147 | 4 | 2.7 |
| Southwest | 213 | 1 | 0.5 |
| Northwest | 99 | 0 | 0 |
| Total | 1,344 | 30 | 2.2 |
| Indicator | Taijiquan group (n = 128) | Control group (n = 121) | P-value |
| ESCA score | 122.5 ± 13.4 | 105.4 ± 12.5 | 0 |
| ADL score | 45.7 ± 6.5 | 39.6 ± 4.8 | 0.007 |
| SF-36 score | 61.5 ± 7.4 | 40.0 ± 5.3 | 0.001 |
| LVEF | 47.3% ± 3.4% | 42.6% ± 3.1% | 0.043 |
| Arrhythmia recovery time, day | 4.5 ± 1.2 | 6.3 ± 1.3 | 0.015 |
| Recovery time of atrioventricular block, day | 3.3 ± 1.6 | 5.5 ± 1.4 | 0.006 |
| Hospital stay, day | 16.4 ± 2.5 | 20.5 ± 4.8 | 0.032 |
| SAS/score | 32.3 ± 4.5 | 43.9 ± 5.6 | 0.001 |
| SDS/score | 39.2 ± 9.3 | 53.6 ± 8.7 | 0.003 |
| Data are presented as mean ± SD. LVEF: left ventricular ejection fraction; SAS: self-rating anxiety scale; SDS: self-rating depression scale. | |||
| Indicators | Control group (n = 135) | Home-based rehabilitation group (n = 135) |
P -value |
| MACE | 12 (8.9%) | 2 ( 1.5%) | 0.002 |
| AMI incidence | 0 | 0 | - |
| Unplanned revascularization | 12 (8.9%) | 2 ( 1.5%) | 0.002 |
| Stroke | 0 | 0 | |
| Cardiac death | 1 (0.6%) | 0 | 0.493 |
| Rehospitalization due to deteriorated angina pectoris | 31 (23%) | 13 (9.7%) | 0.002 |
| Max MET | 5.1 ± 1.4 | 6.2 ± 1.3 | 0.001 |
| VO2peak at anaerobic threshold, mL/kg per minute | 13.7 ± 4.1 | 16.2 ± 4.3 | < 0.001 |
| Systolic pressure, mmHg | 130.1 ± 13.9 | 122.2 ± 13.7 | < 0.001 |
| LDL-C, mmol/L | 2.2 ± 0.8 | 1.5 ± 0.6 | < 0.001 |
| Data are presented as mean ± SD or n (%). CAD: coronary artery disease; LDL-C: low-density lipoprotein cholesterol; MACE: major adverse cardiovascular event. | |||
| Outcomes | Control group ( n = 48) | Intervention group ( n = 49) | P -value |
| VO2peak, mL/kg per minute | 4.9 ± 6.6 | 9.3 ± 8.0 | 0.003 |
| Beliefs related to CVD | 2.5 ± 15.2 | 11.1 ± 10.5 | 0.002 |
| Exercise self-efficacy | 4.2 ± 5.3 | 8.3 ± 4.8 | < 0.001 |
| CVD: cardiovascular diseases. | |||
| Indicator | Early rehabilitation group (n = 192) | Conventional treatment group (n = 192) | P -value |
| Mechanical ventilation duration, h | 36.0 ± 14.9 | 43.0 ± 12.5 | 0.016 |
| Duration of sedative use, h | 39.0 ± 16.8 | 47.0 ± 21.3 | 0.001 |
| Delirium | 15 (7.81%) | 33 (17.19%) | 0.006 |
| Intestinal dysfunction | 51 (26.56%) | 82 (42.71%) | 0.001 |
| Triceps skinfold thickness, mm | 15.0 ± 2.8 | 12.0 ± 3.3 | 0.021 |
| Data are presented as mean ± SD or n (%). | |||
| Group | Hospitalization time/d | Hospitalization cost/CNY |
| Rehabilitation group (n = 200) | 4.2 ± 2.1 | 38,132 ± 9,502 |
| Control group (n = 200) | 6.6 ± 3.2 | 42,867 ± 13,516 |
| P-value | < 0.001 | < 0.001 |
| Data are presented as mean ± SD. | ||
| Release time | Name |
| 2018 | China cardiac rehabilitation and secondary prevention guideline 2018 Essentials[11] |
| 2018 | Chinese expert consensus on exercise rehabilitation of patients with stable CAD aged 75 and above[12] |
| 2020 | Expert consensus on cardiac rehabilitation after CABG[13] |
| 2020 | Chinese expert consensus on cardiac rehabilitation of chronic heart failure[14] |
| 2021 | Chinese expert consensus on cardiac rehabilitation of patients with atrial fibrillation[15] |
| 2021 | Chinese expert consensus on exercise rehabilitation for adult patients with pulmonary hypertension[16] |
| 2022 | Chinese expert consensus on the clinical normative application of 6MWT[17] |
| 2022 | Chinese expert consensus on home-based rehabilitation for patients with cardiovascular diseases[18] |
| CABG: coronary artery bypass grafting; CAD: coronary artery disease. | |