| Citation: | Please cite this article as: Font CM, Fernandez AB, Kadariya D. Unveiling sinus venosus atrial septal defect and partial anomalous pulmonary venous return in an elderly patient. J Geriatr Cardiol 2024; 21(4): 462−464. DOI: 10.26599/1671-5411.2024.04.004. |
Sinus venosus defect (SVD) accounts for 4%–11% of all atrial septal defects (ASD) and may present with dyspnea, heart failure (HF), palpitations, or angina.[1] The malformation typically involves an interatrial communication due to a deficiency in the common wall connecting the right pulmonary veins and the superior vena cava (SVC) and often accompanies anomalous pulmonary venous connection of some or all of the pulmonary veins.[1] Trans-esophageal echocardiography (TEE) is an accurate modality for the diagnosis of SVD.[2] Surgical repair is more complex than repair of secundum ASD,[3] as the patient is at higher risk for residual shunting and stenosis of pulmonary veins or SVC with repair of SVD.[4] The average age at the time of surgical repair in patients with SVD is 8.3 years.[5] This case report describes a 68-year-old female with right HF symptoms who was found to have SVD and partial anomalous pulmonary venous return (PAPVR).
A 68-year-old Caucasian female with a history of pulmonary hypertension (PH), right ventricular dysfunction, severe tricuspid regurgitation, and atrial fibrillation (AF), who previously declined workup for PH and tricuspid regurgitation due to absence of significant symptoms, presented with worsening dyspnea on exertion, lower extremity edema, and abdominal swelling unresponsive to diuretic therapy.
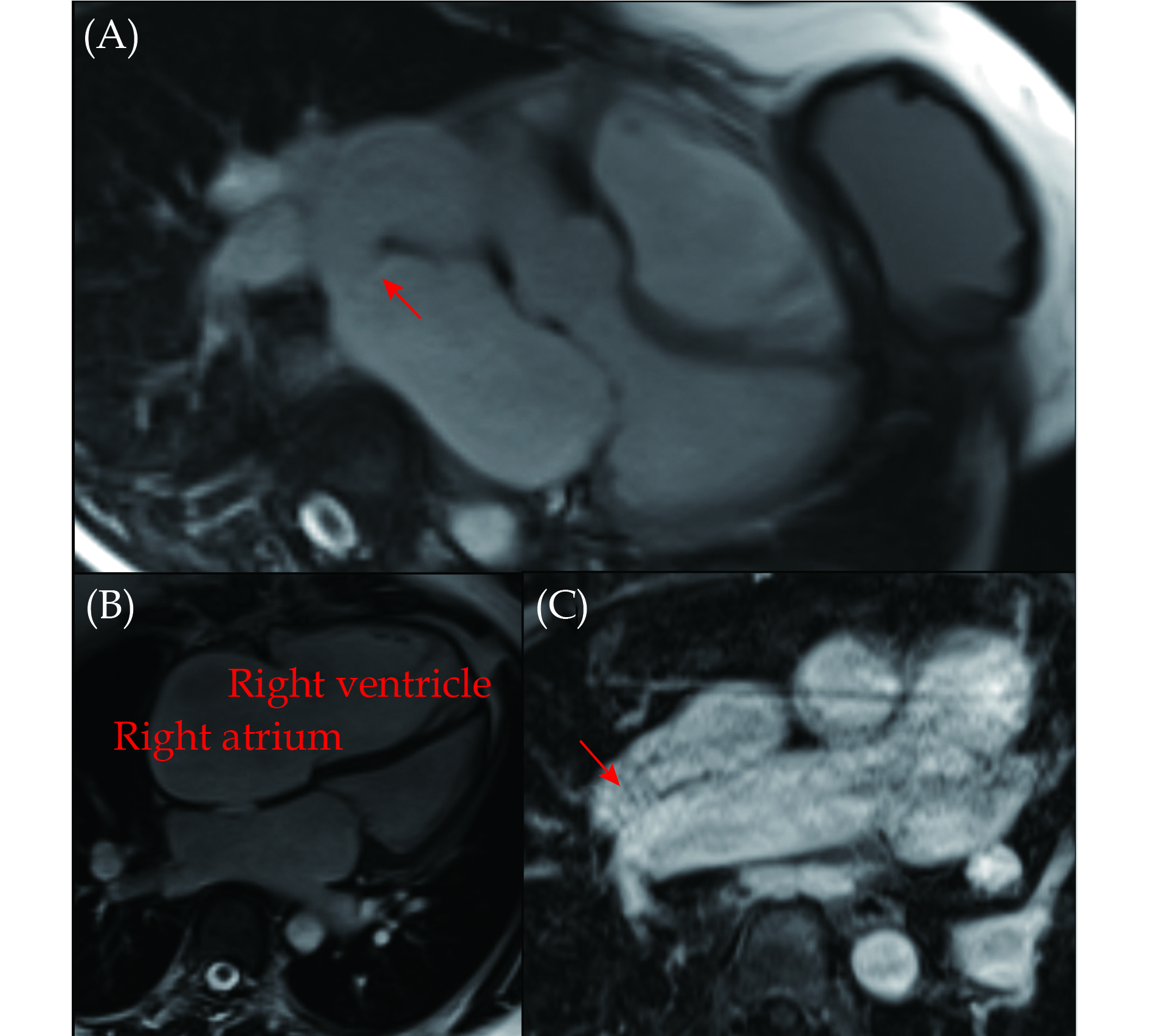
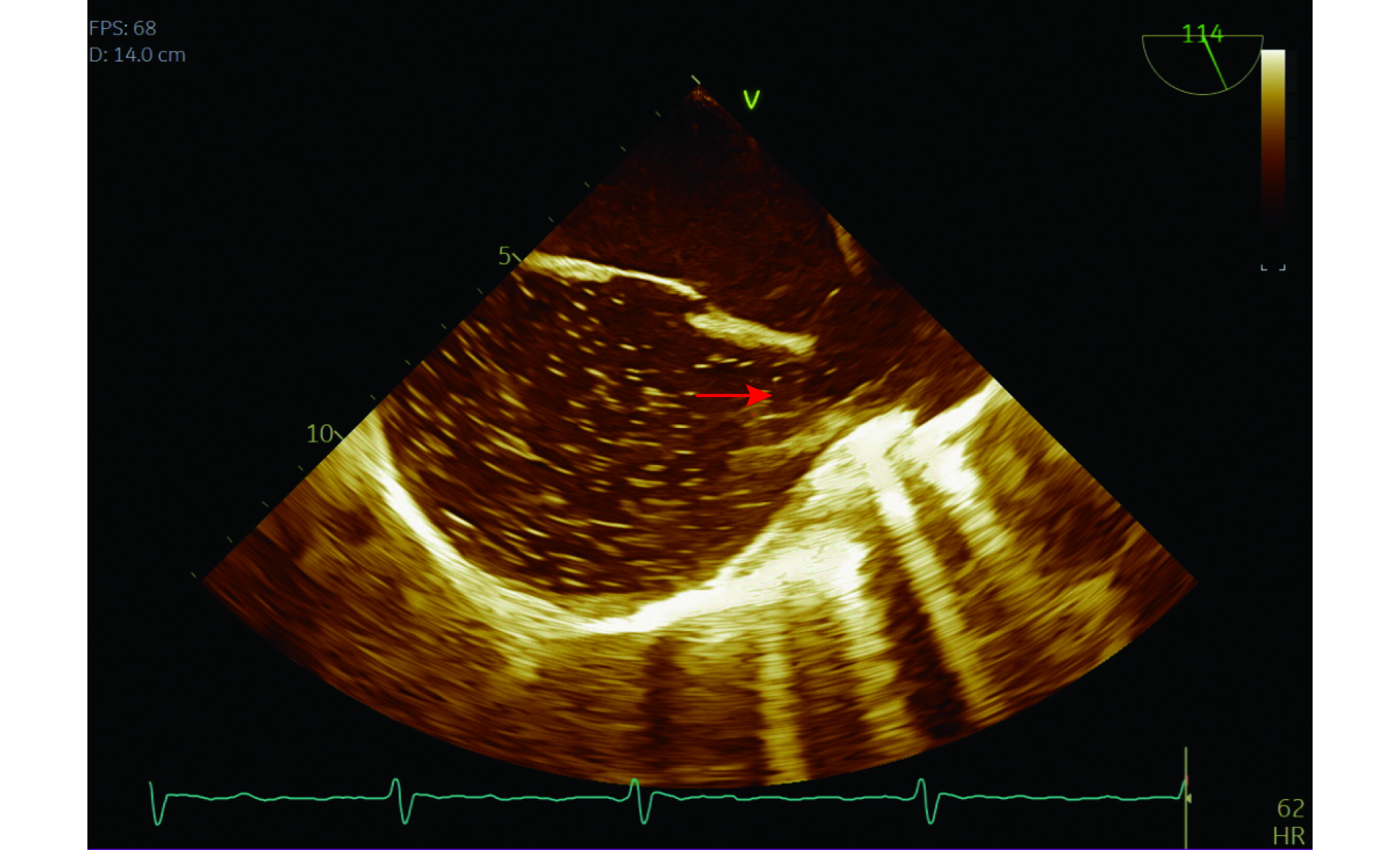
Given unexplained right ventricular dysfunction, a TEE with bubble study was performed to evaluate for intracardiac shunt. This study revealed a superior sinus venosus type ASD with bidirectional shunting, severe right atrial and right ventricular enlargement, and inferior vena cava dilatation (Figure 1). She underwent synchronized cardioversion at this time with successful conversion to sinus rhythm, but returned to AF by the time she was seen in follow up a few months later.
Cardiac magnetic resonance imaging confirmed a large 1.9 cm sinus venosus type ASD (Figure 2A) with large left-to-right shunt ratio (Qp:Qs: 2.34:1) and severely enlarged right ventricle (Figure 2B). It also revealed PAPVR of the right upper pulmonary vein draining to the SVC adjacent to the right atrium (Figure 2C) and an enlarged pulmonary trunk with enlarged left and right main pulmonary arteries. Right heart catheterization showed mild PH, normal cardiac index, and oxygen saturation step up from the SVC to high right atrium (82% to 85%, respectively). Left heart catheterization showed mild nonobstructive coronary artery disease.
Given significant symptoms, was referred for cardiac surgery and underwent repair of sinus venosus ASD and PAPVR using bovine pericardium, tricuspid valve repair using an annuloplasty ring, and ligation of the left atrial appendage. A patent foramen ovale was noted during intraoperative TEE after separating from cardiopulmonary bypass, and this was also surgically closed. Post-procedurally, she was noted to have pacemaker dependence with underlying bradycardia, and a permanent pacemaker was implanted. Echocardiogram post-procedure showed moderately enlarged right ventricle and severely reduced right ventricular systolic function without evidence of tricuspid regurgitation or atrial septal shunting. She was discharged on a small dose of diuretic therapy. She returned to the hospital one week after her discharge due to decompensated HF, and her home diuretic dose was adjusted. At subsequent cardiology office visits, she denied any dyspnea or leg swelling and her volume exam was consistent with euvolemia.
This case illustrates the importance of evaluating for left-to-right intracardiac shunt in patients with unexplained right ventricular dilatation.[2] Surgical repair of this defect can lead to functional improvement, regardless of age at the time of repair.[1] In this elderly patient with a presenting complaint of exertional dyspnea and symptoms of HF, congenital heart disease was an unexpected finding. However, further diagnostic workup including TEE and cardiac magnetic resonance imaging revealed a previously undiagnosed SVD in combination with PAPVR, and the patient did well after surgical repair.
SVD is relatively rare compared to other types of ASD and can present a diagnostic challenge, especially in older adults where clinical suspicion may be low. The atypical location of the defect, near the junction of the SVC and right atrium, can lead to variability in clinical manifestations and diagnostic findings. In this case, the diagnosis was further complicated by the presence of PAPVR, where the right upper pulmonary vein drained anomalously into the SVC, adding to the hemodynamic burden. The clinical significance of ASD and PAPVR lies not only in their potential to cause symptoms but also in their long-term implications for cardiovascular health. Untreated ASD can lead to right heart volume overload, PH, and subsequent right HF, while PAPVR may contribute to pulmonary venous hypertension and further exacerbate right heart strain.[1] Interestingly, despite the advanced age of this patient, she had adapted to her hemodynamic derangements remarkably well, with symptoms presenting late in her life.
In line with current guidelines and after careful consideration of the patient’s age, overall functional status, and severity of symptoms, the decision was made to proceed with surgical repair of the SVD and correction of the associated PAPVR.[6] The patient underwent successful surgical intervention, which involved closure of the atrial defect and redirection of the anomalous pulmonary venous return to the left atrium. Postoperatively, the patient experienced significant improvement in symptoms of exertional dyspnea and fatigue. Follow-up echocardiography confirmed successful closure of the ASD and appropriate redirection of pulmonary venous return. However, she developed sinus node dysfunction, a known complication of SVD repair.[5] Subsequently, she required implantation of a permanent pacemaker.
This case underscores the importance of maintaining a broad differential diagnosis, particularly in elderly patients presenting with nonspecific symptoms. While sinus venosus ASD and PAPVR are relatively uncommon in this age group, they should be considered in the evaluation of unexplained dyspnea and fatigue, as early recognition can lead to appropriate management and improved outcomes through surgical repair, which is effective in relieving symptoms and preventing long-term complications associated with this defect. This case also highlights the multidisciplinary approach required for the management of elderly patients with complex congenital heart disease, involving close collaboration between cardiologists, cardiac surgeons, and, in some cases, electrophysiologists.
Data on long-term outcomes of SVD repair are limited. In a 2005 study examining outcomes of 112 patients undergoing SVD repair, symptomatic improvement was noted in 77% of patients, and patients commonly developed sinus node dysfunction and postoperative AF. The average age at repair was 34 years old, and 15% of patients were aged 61 years and above. Interestingly, clinical improvement was more common with older age at repair; however, older age at surgery was predictive of late mortality and also associated with a higher chance of postoperative AF and postoperative dyspnea.[1] A more recent study in 2024 evaluating outcomes in 182 patients after surgical repair of SVD found that there was no difference in long-term mortality between SVD patients compared with age-matched controls; however the median age of surgical repair in this study was 8.3 years and the majority of patients were under the age of 18 years old.[5] Further research is warranted to better understand the long-term outcomes and optimal timing of surgical intervention in elderly patients with SVD and PAPVR. Additionally, larger studies are needed to evaluate the impact of surgical repair on quality of life and survival in this population.
| [1] |
Attenhofer Jost CH, Connolly HM, Danielson GK, et al. Sinus venosus atrial septal defect: long-term postoperative outcome for 115 patients. Circulation 2005; 112: 1953−1958. doi: 10.1161/CIRCULATIONAHA.104.493775
|
| [2] |
Pascoe RD, Oh JK, Warnes CA, et al. Diagnosis of sinus venosus atrial septal defect with transesophageal echocardiography. Circulation 1996; 94: 1049−1055. doi: 10.1161/01.CIR.94.5.1049
|
| [3] |
Stewart RD, Bailliard F, Kelle AM, et al. Evolving surgical strategy for sinus venosus atrial septal defect: effect on sinus node function and late venous obstruction. Ann Thorac Surg 2007; 84: 1651−1655. doi: 10.1016/j.athoracsur.2007.04.130
|
| [4] |
Russell JL, LeBlanc JG, Deagle ML, et al. Outcome following repair of sinus venosus atrial septal defects in children. Asian Cardiovasc Thorac Ann 2002; 10: 231−234. doi: 10.1177/021849230201000309
|
| [5] |
Muroke V, Jalanko M, Haukka J, et al. Long-term outcome after surgical correction of sinus venosus defect in a nationwide register-based cohort study. Int J Cardiol 2024; 395: 131433. doi: 10.1016/j.ijcard.2023.131433
|
| [6] |
Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019; 73: 1494−1563. doi: 10.1161/CIR.0000000000000602
|