| Citation: | Please cite this article as: Rivas Rios J, ZHANG YX, Oye M, Altunkaynak C, Saremian J, Missov E. New-onset heart failure masking a massive retroperitoneal liposarcoma. J Geriatr Cardiol 2022; 19(4): 319−321. DOI: 10.11909/j.issn.1671-5411.2022.04.003. |
Liposarcoma is one of the most common soft tissue sarcomas, representing 50% of all retroperitoneal sarcomas. A large retroperitoneal sarcoma can exert mass effect on intraabdominal organs and the thoracic cavity producing symptoms similar to those seen in acute decompensated heart failure (HF), such as abdominal swelling, dyspnea on exertion, and orthopnea. However, the presentation with new-onset HF masking a massive retroperitoneal liposarcoma is exceedingly rare. Here, we present an interesting case of an elderly patient with new-onset decompensated HF in the setting of multi-vessel coronary artery disease who responded well to intravenous diuretic therapy without complete symptom resolution. Further workup showed a massive retroperitoneal sarcoma as the contributing etiology. Given his poor cardiac function, he was not initially a surgical candidate. However, after being placed on appropriate goal-directed medical therapy, he experienced recovery in his ejection fraction (EF) and is now a surgical candidate.
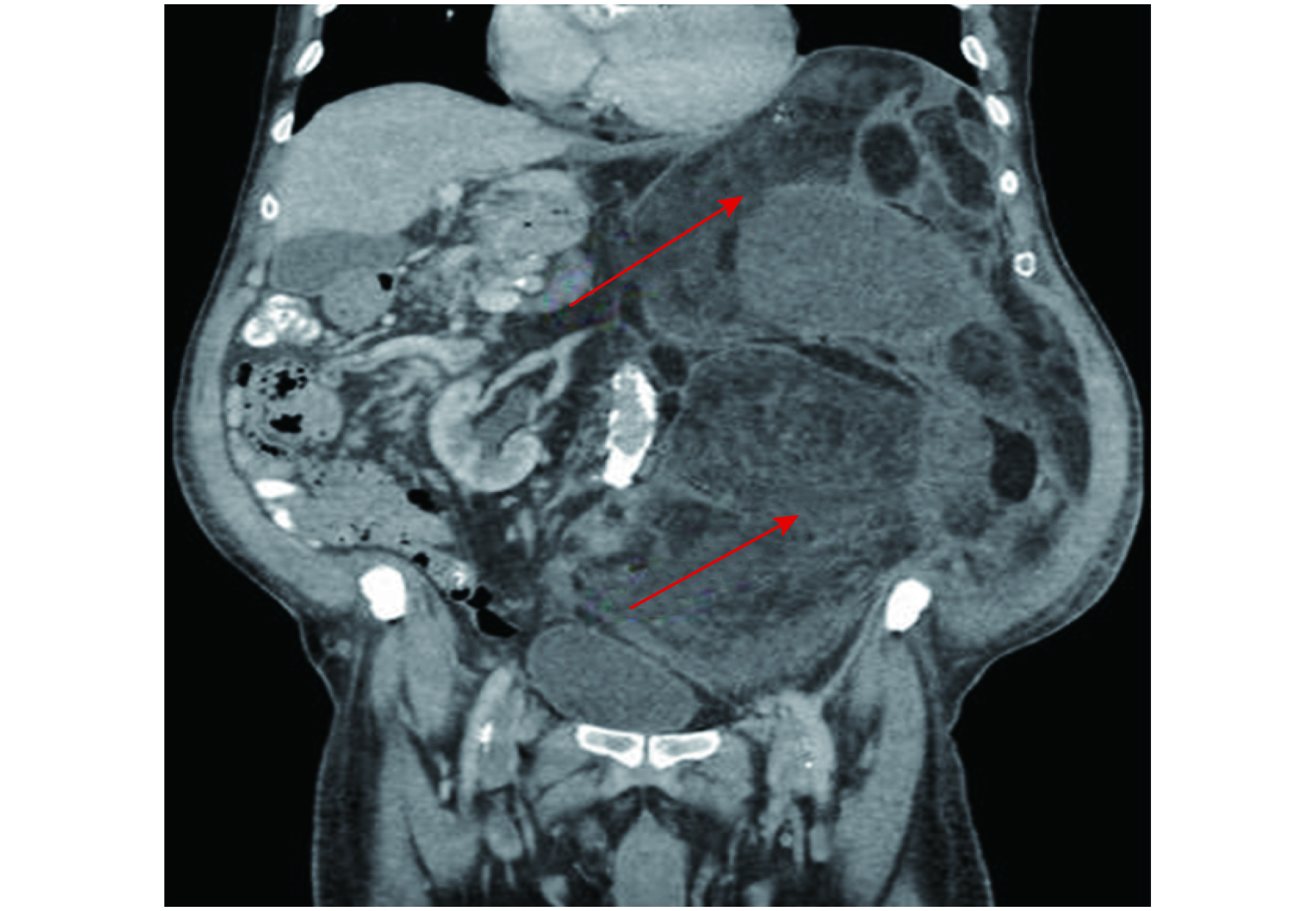
A 78-year-old male with a history of hypertension, hyperlipidemia, and tobacco abuse came to the emergency room with complaints of progressive shortness of breath, orthopnea, and abdominal distention. On initial evaluation, the patient was normotensive, tachycardiac, and volume overloaded. The laboratory results showed elevated N-terminal pro-B-type natriuretic peptide level with a benign comprehensive metabolic panel. Chest X-ray revealed cardiomegaly with pulmonary vascular congestion. Transthoracic echocardiogram showed a severely reduced EF of 10%–15%, left ventricular eccentric hypertrophy and global hypokinesis. He responded well to intravenous diuretics, but had persistent orthopnea and minimal improvement of abdominal distension. He underwent computed tomography of the abdomen and pelvis which showed an extremely bulky, multi-lobulated retroperitoneal mass measuring 29 cm × 33 cm × 35 cm with mass effect on multiple intra-abdominal organs (Figure 1). Computed tomography guided core needle biopsy of the mass confirmed well-differentiated liposarcoma (WDLPS) with atypical spindle cells and adipocytes (Figure 2). Fluorescence in situ hybridization analysis revealed murine double minute 2 (MDM2) amplification. No evidence of metastatic disease was found on additional workup. The patient was not initially a candidate for surgical resection due to his low EF, however, after three months of goal-directed medical therapy, he had recovery in EF from 10%−15% to 40%. Outpatient ischemic evaluation revealed multivessel disease and he underwent coronary artery bypass surgery. He is planned for tumor resection.
Sarcomas are a heterogeneous group of over 80 different tumors arising from mesenchymal or connective tissue. In 2018, soft tissue sarcomas represented approximately 0.8% of all cancers in the United States.[1] Pure WDLS accounts for approximately 40%−50% of liposarcoma and has a male predilection with peak incidence between the fifth and sixth decade of life.[2] WDLS is characterized by chromosome 12q13-15 amplification, which leads to overexpression of a gene called MDM2.[2] MDM2 overexpression is seen nearly universally in WDLS and downregulates the activity of tumor suppressor gene p53.[2] The most common sites of WDLS are the deep muscles of the extremities, followed by the retroperitoneum, and then other sites like the groin and mediastinum.[3] In a review of 92 cases of WDLS, tumors within the retroperitoneum and groin had higher recurrence rates than compared to extremity tumors.[3] Local recurrence is presumably higher within deep spaces because of incomplete resection due to anatomic location.[3]
Our patient presented with classical symptoms of acute decompensated HF that was confirmed by transthoracic echocardiogram with severely reduced EF and global hypokinesis. Since he continued to have orthopnea despite adequate diuresis, further imaging discovered the mass effect of a giant liposarcoma causing mechanical compression of his surrounding organs and into his thoracic cavity resulting in limited diaphragmatic expansion. There is no established association between liposarcoma and HF without metastatic disease, however, there has been a proposition of MDM2’s role in cardiovascular disease.[4] Complete surgical resection remains the preferred treatment method for WDLPS.[5] Adjunctive radiation and chemotherapy have little role in WDLPS, as the tumor is not radiosensitive and there is no established survival benefit from chemotherapy.[6] Given MDM2 over-amplification is consistently seen in WDLPS, molecular-based targeted therapies, such as MDM2 antagonists, are still undergoing clinical trials and research.
In our case, the new-onset systolic HF not only masked a giant retroperitoneal mass on initial evaluation, but also delayed the primary treatment option of surgical resection. This case represents a clinically challenging scenario that required a multidisciplinary team approach. Perhaps, more research can be devoted into the benefit of temporary ventricular assist device perioperatively for non-cardiac surgeries in challenging clinical scenarios.
All authors had no conflicts of interest to disclose.
| [1] |
Gage MM, Nagarajan N, Ruck JM, et al. Sarcomas in the United States: recent trends and a call for improved staging. Oncotarget 2019; 10: 2462−2474. doi: 10.18632/oncotarget.26809
|
| [2] |
Sheth S, Dry S. Well-differentiated/Dedifferentiated liposarcomas: a review with emphasis on recent molecular developments and targeted therapies. Pathol Case Rev 2012; 17: 14−24. doi: 10.1097/PCR.0b013e318246946c
|
| [3] |
Weiss SW, Rao VK. Well-differentiated liposarcoma (atypical lipoma) of deep soft tissue of the extremities, retroperitoneum, and miscellaneous sites. A follow-up study of 92 cases with analysis of the incidence of “dedifferentiation”. Am J Surg Pathol 1992; 16: 1051−1058. doi: 10.1097/00000478-199211000-00003
|
| [4] |
Lam B, Roudier E. Considering the role of murine double minute 2 in the cardiovascular system? Front Cell Dev Biol 2019; 7: 320. doi: 10.3389/fcell.2019.00320
|
| [5] |
Haddox CL, Riedel RF. Recent advances in the understanding and management of liposarcoma. Fac Rev 2021; 10: 1. doi: 10.12703/r/10-1
|
| [6] |
Crago AM, Singer S. Clinical and molecular approaches to well differentiated and dedifferentiated liposarcoma. Curr Opin Oncol 2011; 23: 373−378. doi: 10.1097/CCO.0b013e32834796e6
|
| [1] | Hee-Eun Choi, Chul Kim, Se-Heum Park, Doo-Il Kim, Ki-Hun Kim, Dong-Kie Kim, Seunghwan Kim, Jino Park. Polymorphic ventricular tachycardia during phase II cardiac rehabilitation in a patient with heart failure: a case report[J]. Journal of Geriatric Cardiology, 2020, 17(1): 64-66. DOI: 10.11909/j.issn.1671-5411.2020.01.003 |
| [2] | Yong Hoon Kim, Ae-Young Her, Seung-Woon Rha, Byoung Geol Choi, Se Yeon Choi, Jae Kyeong Byun, Yoonjee Park, Dong Oh Kang, Won Young Jang, Woohyeun Kim, Woong Gil Choi, Tae Soo Kang, Jihun Ahn, Sang-Ho Park, Ji Young Park, Min-Ho Lee, Cheol Ung Choi, Chang Gyu Park, Hong Seog Seo. Calcium channel blocker monotherapy versus combination with renin-angiotensin system inhibitors on the development of new-onset diabetes mellitus in hypertensive Korean patients[J]. Journal of Geriatric Cardiology, 2019, 16(6): 439-447. DOI: 10.11909/j.issn.1671-5411.2019.06.003 |
| [3] | Signe Hoi Rasmussen, Karen Andersen-Ranberg, Jordi Sanchez Dahl, Mads Nybo, Bernard Jeune, Kaare Christensen, Sabine Gill. Diagnosing heart failure in centenarians[J]. Journal of Geriatric Cardiology, 2019, 16(1): 1-11. DOI: 10.11909/j.issn.1671-5411.2019.01.008 |
| [4] | Sarah Birkhoelzer, Daniel Stevens, Donah Zachariah, Jackie Taylor, Nigel Rowell, Paul R Kalra. Ivabradine tolerability in heart failure[J]. Journal of Geriatric Cardiology, 2018, 15(11): 708-709. DOI: 10.11909/j.issn.1671-5411.2018.11.007 |
| [5] | Rubanenko O Anatol´evna, Fatenkov O Veniaminovich, Khokhlunov S Mikhaylovich. Predictors of new-onset atrial fibrillation in elderly patients with coronary artery disease after coronary artery bypass graft[J]. Journal of Geriatric Cardiology, 2016, 13(5): 444-449. DOI: 10.11909/j.issn.1671-5411.2016.05.017 |
| [6] | Bharathi Upadhya, Mark J Haykowsky, Joel Eggebeen, Dalane W Kitzman. Exercise intolerance in heart failure with preserved ejection fraction: more than a heart problem[J]. Journal of Geriatric Cardiology, 2015, 12(3): 294-304. DOI: 10.11909/j.issn.1671-5411.2015.03.013 |
| [7] | Laura Leto, Mauro Feola. Cognitive impairment in heart failure patients[J]. Journal of Geriatric Cardiology, 2014, 11(4): 316-328. DOI: 10.11909/j.issn.1671-5411.2014.04.007 |
| [8] | Azam Torabi, John GF Cleland, Alan S Rigby, Nasser Sherwi. Development and course of heart failure after a myocardial infarction in younger and older people[J]. Journal of Geriatric Cardiology, 2014, 11(1): 1-12. DOI: 10.3969/j.issn.1671-5411.2014.01.002 |
| [9] | Marzia Rigolli, Gillian A Whalley. Heart failure with preserved ejection fraction[J]. Journal of Geriatric Cardiology, 2013, 10(4): 369-376. DOI: 10.3969/j.issn.1671-5411.2013.04.011 |
| [10] | Harsha V. Ganga, Sanjeev U. Nair, Venkata K. Puppala, Wayne L. Miller. Risk of New-Onset Atrial Fibrillation in Elderly Patients with the Overlap Syndrome: A Retrospective Cohort Study[J]. Journal of Geriatric Cardiology, 2013, 10(2): 129-134. DOI: 10.3969/j.issn.1671-5411.2013.02.001 |