| Citation: | Please cite this article as: Acibuca A, Yilmaz M, Karadeli E, Canpolat ET, Erol T. A case of mediastinal mesenchymal tumor resembling hemopericardium. J Geriatr Cardiol 2021; 18(7): 591−594. DOI: 10.11909/j.issn.1671-5411.2021.07.007. |
Mediastinal tumors are rare, comprising 3% of all thoracic neoplasms.[1] Although mediastinal lesions are expected to have a peak incidence in 60 to 70-year-old patients, their overall prevalence in the elderly is very low.[2] An important feature in elderly patients with mediastinal disorders is that they can be asymptomatic. If clinical symptoms do appear, they commonly occur due to invasion or compression of the mass and can range from dyspnea or cough to dysphagia or swelling. Severe compression of the heart can even lead to hypotension.[3] Due to the symptoms overlapping with cardiac diseases, a differential diagnosis of mediastinal neoplasms is challenging, especially in older patients who are more likely to have cardiovascular disorders. The mainstay of the diagnostic process for mediastinal lesions is clinical suspicion, followed by multimodality imaging. Supporting the above-mentioned data, the current case is of an elderly patient with a mediastinal tumor misdiagnosed as hemopericardium.
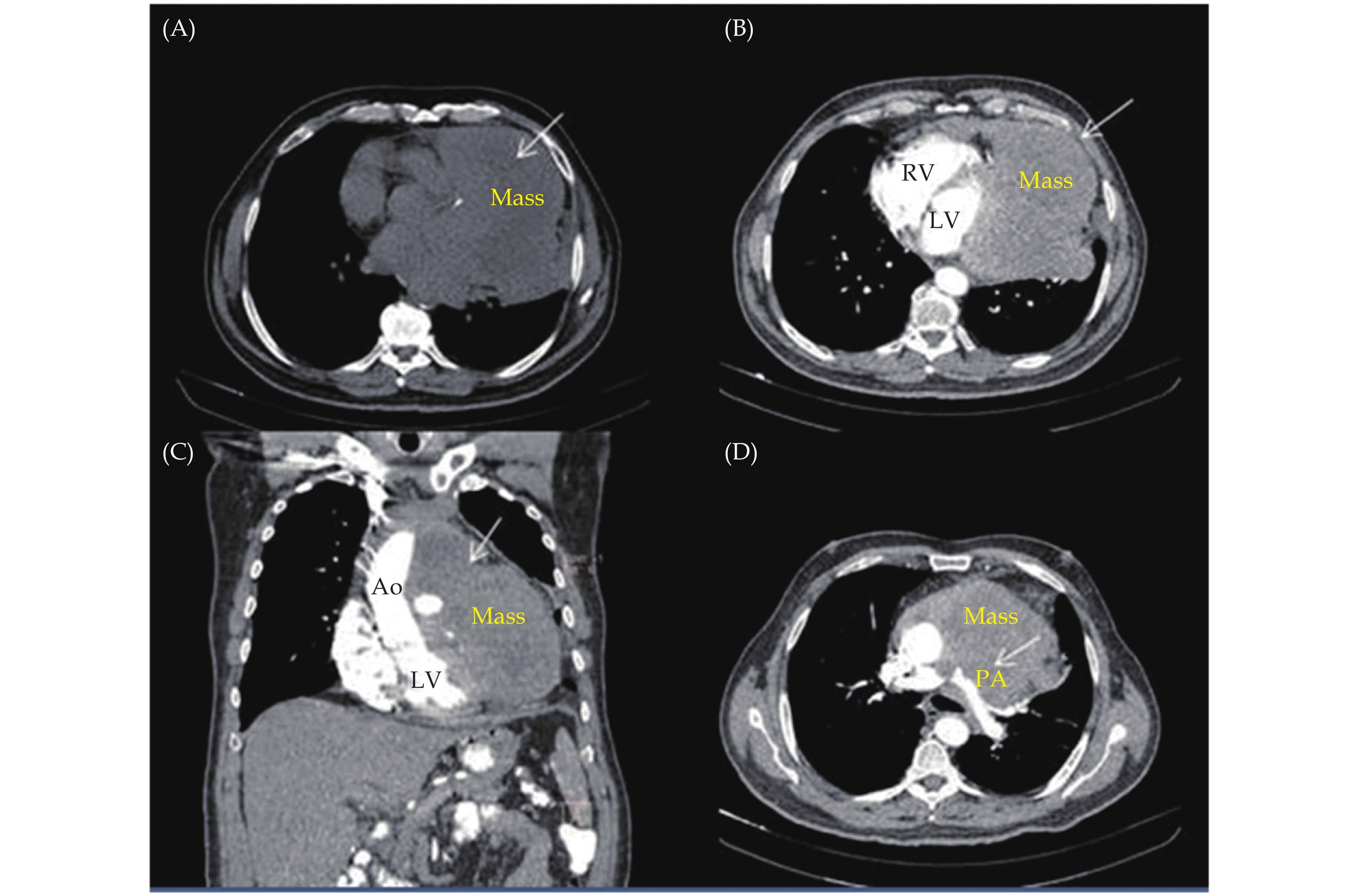
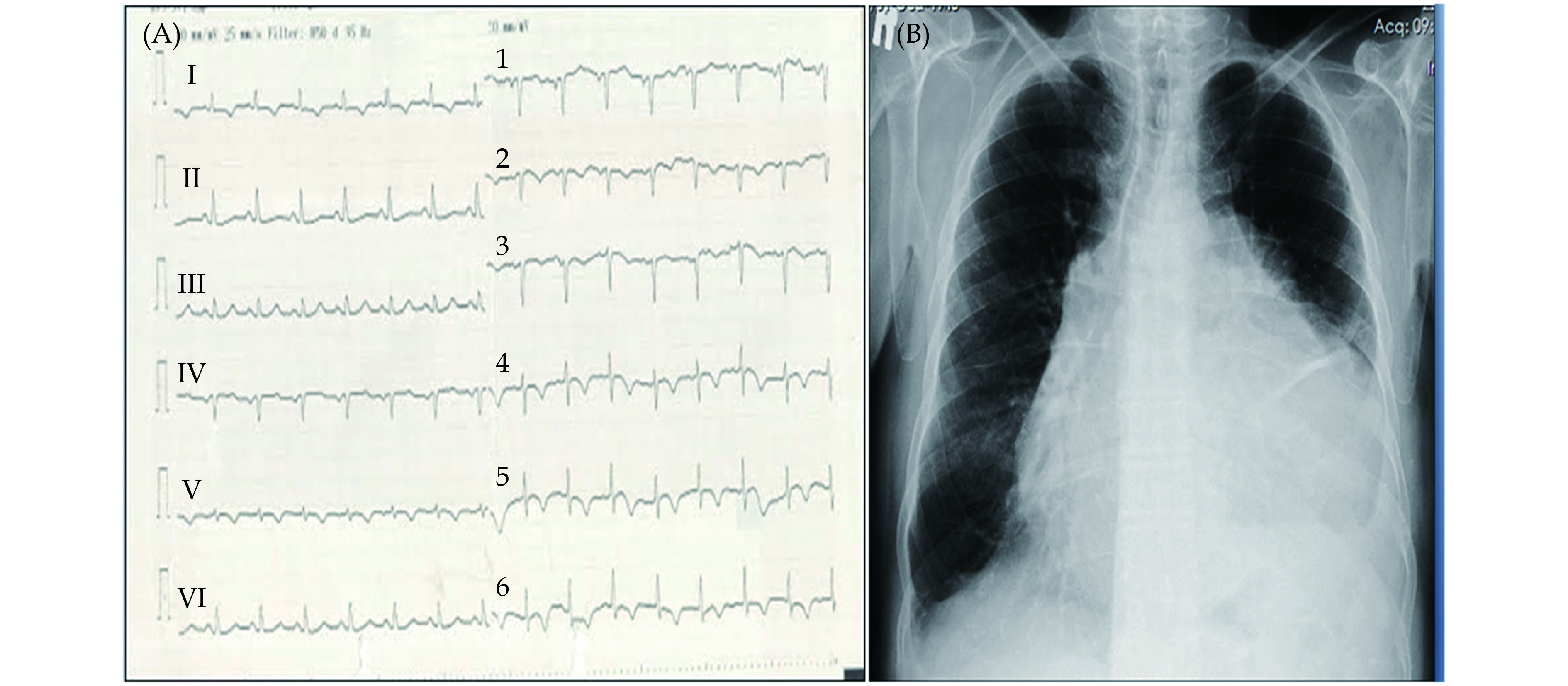
A 74-year-old male with no known disease but who was an ex-smoker was admitted to our hospital with a one-month history of dyspnea and weight loss. Electrocardiography showed negative T waves on the anterior leads (Figure 1A), and a chest X-ray revealed cardiomegaly (Figure 1B). A thoracic computed tomography (CT) was performed because of shortness of breath, and the report showed massive hemorrhagic pericardial effusion. With this finding, an emergency transthoracic echocardiography was performed, and it was considered that it might not be pericardial effusion but a paracardiac mass. Therefore, thoracic and abdominal CTs with contrast were requested, and from this, it was observed that a mediastinal mass was invading and compressing pulmonary vasculatures, the aorta, and the myocardium (Figure 2A–D). There was no sign of primary visceral cancer. Detailed transthoracic echocardiography showed the presence of a hyperechogenic mass compressing the heart and reducing left ventricular functions due to invasion (Video 1–3). Blood tests showed microcytic hypochromic anemia (Hb: 11.48 g/dL) and elevated C-reactive protein (109.3 mg/L). During the follow-up period in the thoracic surgery outpatient clinic for biopsy planning, the patient developed chest pain. His troponin level increased from 230 ng/L to 2143 ng/L (normal range: 0−34.20 ng/L). Coronary angiography was performed, which showed atherosclerotic changes and collaterals vasculating the mass (Video 4–5).
The location was considered inappropriate for a percutaneous biopsy, so a surgical biopsy was performed. The frozen section biopsy revealed a mesenchymal tumor, but the mass was inoperable as there it had invaded the heart and major vasculature. While waiting for the histopathology and immunohistochemistry results, the patient died of sudden cardiac arrest. There had been no progressive deterioration or cardiac arrhythmia. The death was assumed to have resulted from the mass placing severe pressure on the heart chambers, possibly causing them to collapse. Subsequently, the microscopic examination showed mesenchymal spindle cells with mitosis, positive for actin and negative for vimentin, CD34, and S-100. It seemed to be an undifferentiated carcinoma.[4]
The case described here is of a mediastinal mass mimicking an intrapericardial hemorrhage. While the chest X-ray and non-contrast thoracic CT suggested hemorrhagic pericardial effusion, the echocardiographic results and medical history raised enough suspicion for an investigation into a diagnosis other than hemopericardium. It is a fact that mediastinal tumors are mostly asymptomatic and usually diagnosed incidentally during thoracic imaging for other reasons.[5]
The diagnostic process of mediastinal enlargement should begin with a detailed medical history and should be supported by imaging modalities. In the case presented, a malignant disease was suspected because of the patient’s weight loss and older age. A thoracic CT with contrast can differentiate mediastinal neoplasms from other intrathoracic diseases, and detailed data can be obtained about the tumor’s dimension, location, and proximity to organs. On the other hand, the accessibility of CTs or possible limitations in the use of ionic agents can prevent clinicians from obtaining tomographic images. In such a situation, echocardiography can supply valuable clinical data in a more favorable and easy manner. This case highlights the importance of echocardiographic imaging for the rapid and accurate differentiation of mediastinal diseases.
Similar to the case presented, Chamsi-Pasha, et al.[6] reported a patient with a yolk sac tumor in the anterior mediastinum, resembling pericardial effusion. In this case, while attempting pericardiocentesis, no pericardial effusion was encountered. They noted that unsuccessful attempts at pericardial effusion aspiration should be a clue for the diagnosis of paracardiac masses. They also suggested keeping in mind the absence of the “swinging heart” motion in cases of massive effusion to rule out intrapericardial accumulation. The report also discussed previous cases of mediastinal angiosarcoma, mesothelioma, and teratoma, each of which mimicked pericardial effusion. In addition, Jayaprakash, et al.[7] reported a case of a large pericardial mass resembling pericardial effusion, which also described an unsuccessful attempt at pericardial effusion aspiration.
In conclusion, the diagnosis of mediastinal tumors can be confused with pericardial fluid accumulation because of overlapping symptoms with cardiac diseases. Physicians should consider mediastinal masses, despite their rarity, as part of differential diagnosis when mediastinal expansion is seen. Clinical suspicion accompanied by multimodality imaging can prevent inappropriate, invasive procedures such as pericardiocentesis and accelerate the treatment process, which is especially important in older patients prone to fragility and debility. Informed consent for publication of clinical data was obtained from the patient’s relatives.
| [1] |
Shields TW. Overview of primary mediastinal tumors and cysts. In General Thoracic Surgery, 6th Edition; Shields TW, Locicero J, Ponn RB, Rusch VW, Eds.; Lippincott Williams & Wilkins: Philadelphia, USA, 2005; 2489-2493.
|
| [2] |
Liu T, Al-Kzayer LFY, Xie X, et al. Mediastinal lesions across the age spectrum: a clinicopathological comparison between pediatric and adult patients. Oncotarget 2017; 8: 59845−59853. doi: 10.18632/oncotarget.17201
|
| [3] |
Aroor AR, Prakasha S R, Seshadri S, et al. A study of clinical characteristics of mediastinal mass. J Clin Diagn Res 2014; 8: 77−80.
|
| [4] |
Travis WD, Brambilla E, Burke AP, et al. Introduction to the 2015 World Health Organization Classification of Tumors of the Lung, Pleura, Thymus, and Heart. J Thorac Oncol 2015; 10: 1240−1242. doi: 10.1097/JTO.0000000000000663
|
| [5] |
Priola AM, Priola SM, Cardinale L, et al. The anterior mediastinum: diseases. Radiol Med 2006; 111: 312−342. doi: 10.1007/s11547-006-0032-5
|
| [6] |
Chamsi-Pasha H, Bernstein A. Mediastinal yolk sac tumour mimicking pericardial effusion. Thorax 1988; 43: 339−340. doi: 10.1136/thx.43.4.339
|
| [7] |
Jayaprakash S, Byrappa S, Prakash SS, Shankar S. Large pericardial mass mimicking pericardial effusion. Heart Views 2017; 18: 106−107. doi: 10.4103/1995-705X.217854
|