| Citation: | Marta Fontes-Oliveira, Maria Trêpa, Patrícia Rodrigues, Preza Fernandes, Sandra Magalhães, Sofia Cabral, Mário Santos, Severo Torres. Cardiovascular rehabilitation in patients aged 70-year-old or older: benefits on functional capacity, physical activity and metabolic profile in younger vs. older patients[J]. Journal of Geriatric Cardiology, 2020, 17(9): 544-553. DOI: 10.11909/j.issn.1671-5411.2020.09.003 |
The positive clinical impact and cost-effectiveness of exercise-based cardiac rehabilitation (EBCR) programs in the secondary prevention of coronary artery disease (CAD) is well recognized.[1] These programs are characterized by a comprehensive approach to reduce cardiovascular risk, including exercise training sessions, promotion of lifestyle changes and psychological support.[2] In addition to their beneficial impact on quality of life, they have been shown to reduce morbidity and mortality in patients with CAD.[2-4] Accordingly, international guidelines strongly recommend that patients who have suffered an acute myocardial infarction (AMI) should be referred to an EBCR.[5, 6]
In developed countries, the increasingly prevalent aging population accounts for about half of the AMI.[7] However, these patients are underrepresented in overall clinical research, [8, 9] as well as in studies looking at cardiac rehabilitation.[10-12] The aging eligible population to EBCR presents challenges to traditional programs because older patients often have reduced functional capacity, higher rates of social isolation, [13] more comorbidities and more severe CAD.[14-16] Albeit different reports concur as to the favorable responses to EBCR in this patient population, [17, 18] participation rates in EBCR among patients aged 70-years-old or more are still below the expected for this growing population, in part due to a low rate of physicians' referral.[19, 20] Other reasons for poor participation in this population may include socioeconomic factors, such as difficulties in transportation to EBCR centers[21] and psychological factors, such denial of the severity of disease and depression.[22] However, the most powerful predictor of EBCR participation is the strength of the primary physician's recommendation.[21] In this study, we aimed at assessing the global impact of an EBCR program on functional capacity, daily physical activity and metabolic profile in ≥ 70-year-old versus younger patients after an AMI.
This study was approved by the local ethics committee (local number 2020.008 (005-DEFI-006-CE)) and was performed in accordance with the revised declaration of Helsinki. Patients' informed consents were waived due to the retrospective observational design of the study and because all records were anonymized.
We retrospectively evaluated consecutive patients who completed an EBCR program between 2008 and 2017 after a hospitalization for AMI at our hospital. Older patients were defined by age ≥ 70 years. Although there are several cut-offs proposed to define elderly people, we believe that at the current decade this cut-off is most appropriate. Patients between 60 and 69-years-old frequently still work and have similar lifestyles to younger patients, while when they reach 70-years-old, most patients have already retired. We also tested higher age cut-offs, but the percentage of older patients would significantly decrease and limit the analysis (2.3% were ≥ 80 and 8.3% of patients were ≥ 75-years-old). Patients' clinical history, including cardiovascular risk factors, was collected by electronic health records review.
Of the initial 2551 patients referred to EBCR (585 aged ≥ 70 years), we excluded those who were referred to the EBCR program for other reason than an AMI (Supplemental Figure 1). Of the remaining 1995 patients (440 aged ≥ 70 years), we included patients who completed the EBCR, excluding those who for some reason did not finish the program (388 patients).
Patients underwent an EBCR which started during hospital stay (phase 1) and continued through the first year after the AMI (phases 2 and 3). This study specifically focuses on the impact of the EBCB phase 2.
Phase 1 of the EBCR began during hospitalization with supervised sessions of low intensity exercises and counselling with respect to the patients' condition and associated lifestyle changes.
Phase 2 started within two weeks after hospital discharge and took place in the Rehabilitation Unit of our tertiary university hospital. Blood analysis and a symptom-limited exercise stress test (on a treadmill) were performed at baseline and at the end of EBCR phase 2. Bruce protocol (and modified Bruce protocol when considered adequate) were used for the exercise treadmill test.
Exercise prescription was individualized based on clinical data and stratification of cardiac risk, according to the international recommendations.[23] Following this initial evaluation, patients underwent a supervised exercise training protocol of bi-weekly sessions during a period of 6-12 weeks. The number of sessions was similar for both younger and older patients. The training protocol consisted of four parts: 10 min of warm-up, 40 min of aerobic training, 15 min of resistance training and 10 min of cool-down and flexibility exercises. The intensity of aerobic exercise was individually prescribed to a target heart rate (HR) calculated by the Karvonen formula [target training HR = resting HR + (peak HR– resting HR) × intensity level], [24] using the peak HR obtained from the stress treadmill test, complemented by the patient's perceived exertion by Borg's scale.[25, 26] Additionally, patients were also encouraged to maintain exercise activity on days free from EBCR sessions.
The second phase of this EBCR program also included group education sessions on CAD and individual counselling for cardiovascular risk factors control. Social support, nutrition, smoking cessation, endocrinology, urology, vascular surgery and psychiatry support were offered when considered necessary.
Phase 3 of the program started after the supervised hospital-EBCR program. During this phase, patients were encouraged to maintain a healthy lifestyle and to perform ambulatory exercise activities.
During the EBCR program, clinical assessment, blood analysis and symptom-limited exercise stress testing (on a treadmill) were performed before, at the end of phase 2 of the EBCR program and at 12 months. These data are collected in a standardised fashion for every patient who completes the CRP, and the data are entered in a prospective database.
In this study, we examined the evolution of multiple variables [functional capacity, daily physical activity, total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglycerides and glycated haemoglobin (HbA1c), the prognostic biomarker NT-pro-brain natriuretic peptide (NT-pro-BNP), and high-sensitivity C-reactive protein] before and after the second phase of the EBCR program in both young and older patients.
The primary outcomes of this study were the change on functional capacity, daily physical activity and metabolic profile in patients ≥ 70-years-old between baseline and after the EBCR program. The secondary outcome was the comparison between changes in older and younger patients.
Functional capacity was assessed by metabolic equivalents of task (METs)-1 MET corresponding to the consumption of 3.5 mL O2/kg per min—calculated from a symptom limited exercise treadmill test.[26] Body mass index was calculated from the formula weight (kg)/height (m2). Patients' daily physical activity was estimated using the International Physical Activity Questionnaire (IPAQ), [27] a survey already validated in the Portuguese population for this purpose.[28] The IPAQ score is expressed as METs—minutes/week. Patients with a score higher than 3000 are considered to be highly active, and a score below 600 is considered to be inactive.
Echocardiographic data was derived from the transthoracic echocardiogram performed before discharge during the AMI-related hospitalization. Left ventricle ejection fraction was calculated using either eyeballing or the biplane Simpson method according to the guidelines.[29] Glomerular filtration rate was calculated using the Chronic Kidney Disease Epidemiology Collaboration (EPI-CKD) equation.[30]
Histograms were used to assess normality of distribution of the data. Continuous variables are expressed as mean ± SD for normally distributed data or median (interquartile range) for non-normally distributed data. Categorical variables are expressed in absolute values and proportion (n (%)). Comparisons between the younger versus older groups of patients were performed using 2-sided unpaired t-tests or Wilcoxon rank sums test for normally and non-normally distributed data, respectively, or χ2 tests to compare proportions. Parameter comparison between before and after CRP was performed using paired t-test for parametric or Wilcoxon matched-pairs signed-rank test for non-parametric data, as appropriate.
Linear regression was performed to assess the effect of age as a continuous variable in the evolution of the analysed parameters—IPAQ score, NT pro-BNP and C reactive protein variables were log transformed for this purpose. Adjustment for potential confounders was performed using multiple linear regression including the baseline characteristics which were significantly different (P < 0.05) between both age groups.
Statistical analysis was performed using Stata software Version 14.1 (Stata Corp LP, College Station, TX, USA). A two-sided P-value < 0.05 was considered significant.
Clinical and demographic characteristics of the study population are summarized in Table 1. A total of 1607 patients attended our EBCR program after an AMI between 2008 and 2017. Most patients were male (81%) and 333 patients (21%) were aged ≥ 70-years-old. Dyslipidaemia (69%), hypertension (57%) and obesity (50%) were the most common cardiovascular risk factors. Most patients were considered inactive according to the IPAQ score.
| All patients (n = 1607) | < 70 years old (n = 1274) | ≥ 70 years old (n = 333) | P-value | |
| Age, yrs | 60.4 ± 10.3 | 56.8 ± 8.1 | 74.3 ± 3.1 | < 0.001 |
| Gender, female | 19.4% | 18.5% | 22.8% | 0.08 |
| Hypertension | 57.0% | 52.8% | 73.0% | < 0.001 |
| Diabetes mellitus | 33.4% | 32.4% | 37.4% | 0.14 |
| Dyslipidemia | 68.9% | 68.5% | 70.2% | 0.56 |
| Smoking | ||||
| Current smoker | 38.7.7% | 44.8% | 16.2% | < 0.001 |
| Past smoker | 12.0% | 12.9% | 8.4% | |
| Obesity | 49.5% | 50.1% | 47.4% | 0.39 |
| BMI, kg/m2 | 26.3 ± 3.8 | 26.4 ± 3.9 | 25.8 ± 3.6 | 0.02 |
| Abdominal perimeter, cm | 97.2 ± 9.9 | 96.9 ± 9.9 | 98.0 ± 9.8 | 0.07 |
| Multivessel disease | 66.1% | 64.2% | 73.1% | 0.02 |
| 3-vessel disease | 34.1% | 32.8% | 39.2% | |
| STEMI | 35.8% | 39.0% | 26.1% | 0.11 |
| Moderate LVSD | 9.9% | 11.1% | 5.3% | 0.39 |
| Severe LVSD | 6.0% | 5.3% | 8.6% | |
| NT pro-BNP, ng/mL | 457 (210–1064) | 410 (190–901) | 838 (280–1722) | < 0.001 |
| Glomerular filtration rate, mL/min | 67.3 ± 27.1 | 70.4 ± 27.3 | 55.5 ± 23.3 | < 0.001 |
| Marital status | ||||
| Married/living with partner | 81.4% | 82.3% | 77.9% | |
| Single | 5.4% | 5.8% | 3.7% | < 0.001 |
| Divorced | 7.3% | 8.3% | 3.7% | |
| Widowed | 5.9% | 3.5% | 14.8% | |
| β-blockers | 81.6% | 84.6% | 70.2% | < 0.001 |
| ACEI or ARB | 62.6% | 61.3% | 67.8% | 0.06 |
| Statins | 95.9% | 96.5% | 93.9% | 0.07 |
| Diuretics | 17.3% | 15.3% | 24.9% | < 0.001 |
| Calcium channel blockers | 11.1% | 9.4% | 17.4% | 0.001 |
| Nitrates | 19.5% | 17.8% | 25.7% | 0.005 |
| Total cholesterol, mg/dL | 174.6 ± 41.2 | 177.4 ± 41.7 | 163.5 ± 37.1 | < 0.001 |
| HDL-C, mg/dL | 40.7 ± 11.7 | 40.4 ± 0.3 | 42.3 ± 0.6 | 0.008 |
| LDL-C, mg/dL | 105.8 ± 34.8 | 108.0 ± 35.2 | 97.1 ± 32.0 | < 0.001 |
| Triglycerides, mg/dL | 144.5 ± 85.2 | 149.7 ± 90.1 | 124.3 ± 58.1 | < 0.001 |
| HbA1c, % | 6.3 ± 1.3 | 6.3 ± 1.3 | 6.3 ± 1.0 | 0.32 |
| CRP, mg/dL | 5.7 (2.4-12.2) | 5.7 (2.5-12.2) | 5.3 (2.4-12.5) | 0.47 |
| Functional capacity (METs) | 8.6 ± 2.3 | 9.0 ± 2.3 | 7.0 ± 1.9 | < 0.001 |
| IPAQ | 0 (0-693) | 0 (0-693) | 0 (0-693) | 0.94 |
| Data are presented as mean ± SD or median (interquartile range) unless other indicated. ACEI: angiotensin-converting enzyme inhibitors; ARB: angiotensin receptor blockers; BMI: body mass index; CRP: C-reactive protein; HbA1c: glycated haemoglobin; HDL-C: high-density lipoprotein cholesterol; IPAQ: International Physical Activity Questionnaire; IQR: interquartile range; LDL-C: low-density lipoprotein cholesterol; LVSD: left ventricle systolic dysfunction; MET: metabolic equivalenttask; NT pro-BNP: NT pro-brain natriuretic peptide; STEMI: ST-segment elevation myocardial infarction. | ||||
Older patients had a higher prevalence of hypertension (73% vs. 53%, P < 0.001), worse renal function (glomerular filtration rate: 63.8 ± 35.5 vs. 79.1 ± 43.7 mL/min per 1.73 m2, P < 0.001), better lipid profile (total cholesterol: 163.5 ± 37.1 vs. 177.4 ± 41.7 mg/dL, P < 0.001; HDL-C: 42.3 ± 0.6 vs. 40.4 ± 0.3 mg/dL, P = 0.008; LDL-C: 97.1 ± 32.0 vs. 108.0 ± 35.2 mg/dL, P < 0.001; TG: 124.3 ± 58.1 vs. 149.7 ± 90.1 mg/dL, P < 0.001), and were less likely to be smokers (current or past) than their younger counterparts (25% vs. 58% respectively, P < 0.001). Older individuals also presented multivessel CAD more frequently (73% vs. 64%, P = 0.015) and had higher NT-pro-BNP levels (838 [280-1722] vs. 410 [190-901] ng/mL, P < 0.001). Older patients were less likely to live with their partner with a greater percentage of widowed patients (15% vs. 4%, P < 0.001). Significant differences were also present in the prescription of diuretics, calcium channel blockers, nitrates (26% vs. 18%, P = 0.005) and beta-blockers (Table 1). As expected, older patients had a significantly lower baseline functional capacity (7.0 ± 1.9 vs. 9.0 ± 2.3 METs, P < 0.001).
After a phase Ⅱ EBCR program, an overall improvement in several parameters was observed, in both younger and older patients (Table 2). Functional capacity increased from 8.6 ± 2.3 to 10.0 ± 2. 3 METs, P < 0.001 and daily physical activity measured by the IPAQ score increased from low to moderate physical activity (0 [0-693] to 1386 [990-2142], P < 0.001). Metabolic profile also improved, with a significant reduction in body mass index (26.3 ± 3.8 vs. 25.8 ± 3.7 kg/m2, P < 0.001), abdominal perimeter (97.2 ± 9.9 vs. 94.4 ± 10.2 cm, P < 0.001), LDL-C (105.8 ± 34.8 vs. 80.9 ± 28.5 mg/dL, P < 0.001) and TG (144.5 ± 85.2 vs. 117.8 ± 58.1 mg/dL, P < 0.001), an increase in HDLc cholesterol (40.7 ± 11.7 vs. 44.4 ± 12.1 mg/dL, P < 0.001) and an improvement in HbA1c (6.3 ± 1.3 vs. 609 ± 1.0%, P < 0.001). A significant reduction in NT-pro-BNP was observed during this period (457 [210-1064] vs. 242 [106-562] ng/mL, P < 0.001). Inflammation, measured by C-reactive protein, was also reduced after the EBCR program (5.7 [2.45-12.15] vs. 1.8 [0.90-3.41] mg/mL, P < 0.001). After a phase Ⅱ EBCR program, most smokers quit smoking, and the ones who continued to smoke, significantly reduced the number of cigarettes smoked per day (Table 2).
| Characteristic | All patients (n = 1607) | < 70 years old (n = 1274) | ≥ 70 years old (n = 333) | |||||||||||
| Baseline | After EBCR | Delta Δ | P value | Baseline | After EBCR | Delta Δ | P value | Baseline | After EBCR | Delta Δ | P value | |||
| Functional capacity (METs) | 8.6 ± 2.3 | 10.0 ± 2.3 | 1.4 ± 1.2 | < 0.001 | 9.0 ± 2.3 | 10.4 ± 2.2 | 1.5 ± 1.2 | < 0.001 | 7.0 ± 1.9 | 8.4 ± 2.0 | 1.4 ± 1.2 | < 0.001 | ||
| IPAQ | 0 (0-693) | 1386 (990-2142) | 1094 (594-1533) | < 0.001 | 0 (0-693) | 1386 (1040-2384) | 1200 (693-1680) | < 0.001 | 0 (0-693) | 1386 (693-1434) | 693 (396-1386) | < 0.001 | ||
| BMI, kg/m2 | 26.3 ± 3.8 | 25.8 ± 3.7 | -0.6 ± 1.0 | < 0.001 | 26.4 ± 3.9 | 25.9 ± 3.8 | -0.5 ± 1.0 | < 0.001 | 25.8 ± 3.6 | 25.2 ± 3.5 | -0.6 ± 0.8 | < 0.001 | ||
| Abdominal perimeter, cm | 97.2 ± 9.9 | 94.4 ± 10.2 | -2.8 ± 5.8 | < 0.001 | 96.9 ± 9.9 | 94.2 ± 10.1 | -2.7 ± 5.6 | < 0.001 | 98.0 ± 9.8 | 95.1 ± 10.6 | -2.9 ± 6.5 | < 0.001 | ||
| Total cholesterol, mg/dL | 174.6 ± 41.1 | 147.6 ± 35.2 | -29.7 ± 42.1 | < 0.001 | 177.4 ± 41.7 | 147.3 ± 34.6 | -33.0 ± 42.8 | < 0.001 | 163.5 ± 37.1 | 148.7 ± 37.6 | -16.2 ± 36.0 | < 0.001 | ||
| HDL-C, mg/dL | 40.7 ± 11.7 | 44.4 ± 12.1 | 2.2 ± 9.1 | < 0.001 | 40.4 ± 0.3 | 43.1 ± 12.0 | 2.0 ± 9.2 | < 0.001 | 42.3 ± 0.6 | 46.8 ± 12.0 | 3.1 ± 8.1 | 0.001 | ||
| LDL-C, mg/dL | 105.8 ± 34.8 | 80.9 ± 28.5 | -27.4 ± 35.5 | < 0.001 | 108.0 ± 35.2 | 80.6 ± 27.6 | -30.2 ± 35.8 | < 0.001 | 97.1 ± 32.0 | 82.2 ± 31.7 | -16.3 ± 32.1 | 0.0001 | ||
| Triglycerides, mg/dL | 144.5 ± 85.2 | 117.8 ± 58.1 | -30.0 ± 75.5 | < 0.001 | 149.7 ± 90.1 | 120.2 ± 61.0 | -33.0 ± 80.2 | < 0.001 | 124.3 ± 58.1 | 108.2 ± 44.3 | -18.2 ± 51.4 | 0.0181 | ||
| HbA1c, % | 6.3 ± 1.3 | 6.0 ± 1.0 | -0.4 ± 0.8 | < 0.001 | 6.3 ± 1.3 | 6.0 ± 1.0 | -0.4 ± 0.8 | < 0.001 | 6.3 ± 1.0 | 6.1 ± 0.9 | -0.3 ± 0.6 | < 0.001 | ||
| NT pro-BNP, ng/mL | 457 (210-1064) | 242 (106-562) | -201 (514--41) | < 0.001 | 410 (190-901) | 217 (93-511) | -189 (451--38) | < 0.001 | 838 (280-1722) | 412 (190-1016) | -321 (-914--68) | < 0.001 | ||
| CRP, mg/dL | 5.7 (2.4-12.2) | 1.8 (0.9-3.4) | -3.7 (-9.6--0.7) | < 0.001 | 5.7 (2.5-12.2) | 1.8 (0.9-3.5) | -3.6 (-9.6--0.8) | < 0.001 | 5.3 (2.4-12.5) | 2.0 (1.2-3.1) | -3.9 (-9.8--0.6) | < 0.001 | ||
| Glomerular filtration rate, mL/min | 76.0 ± 42.6 | 65.6 ± 28.0 | -10.7 ± 28.1 | < 0.001 | 79.1 ± 43.7 | 68.4 ± 28.7 | -11.0 ± 29.0 | < 0.001 | 63.8 ± 35.5 | 54.6 ± 21.4 | -9.3 ± 24.5 | < 0.001 | ||
| Current smokers, % | 38.7 | 13.3 | -25.4 | < 0.001 | 44.8 | 14.3 | -30.5 | < 0.001 | 16.2 | 9.6 | -6.6 | < 0.001 | ||
| Cigarettes / day, n* | 20 (10-30) | 5 (3-10) | -9 (19-0) | < 0.001 | 20 (10-30) | 5 (3-10) | -9 (19-0) | < 0.001 | 20 (15-35) | 7 (4-8) | -4 (-18--2) | < 0.001 | ||
| Data are presented as mean ± SD or median (interquartile range) unless other indicated. BMI: body mass index; CRP: C-reactive protein; EBCR: exercise-based cardiac rehabilitation; HbA1c: glycated haemoglobin; HDL-C: high-density lipoprotein cholesterol; IPAQ: International Physical Activity Questionnaire; LDL-C: low-density lipoprotein cholesterol; METs: metabolic equivalents; NT-pro-BNP: NT pro-brain natriuretic peptide; *Cigarettes/day from patients who continued to smoke after EBCR. | ||||||||||||||
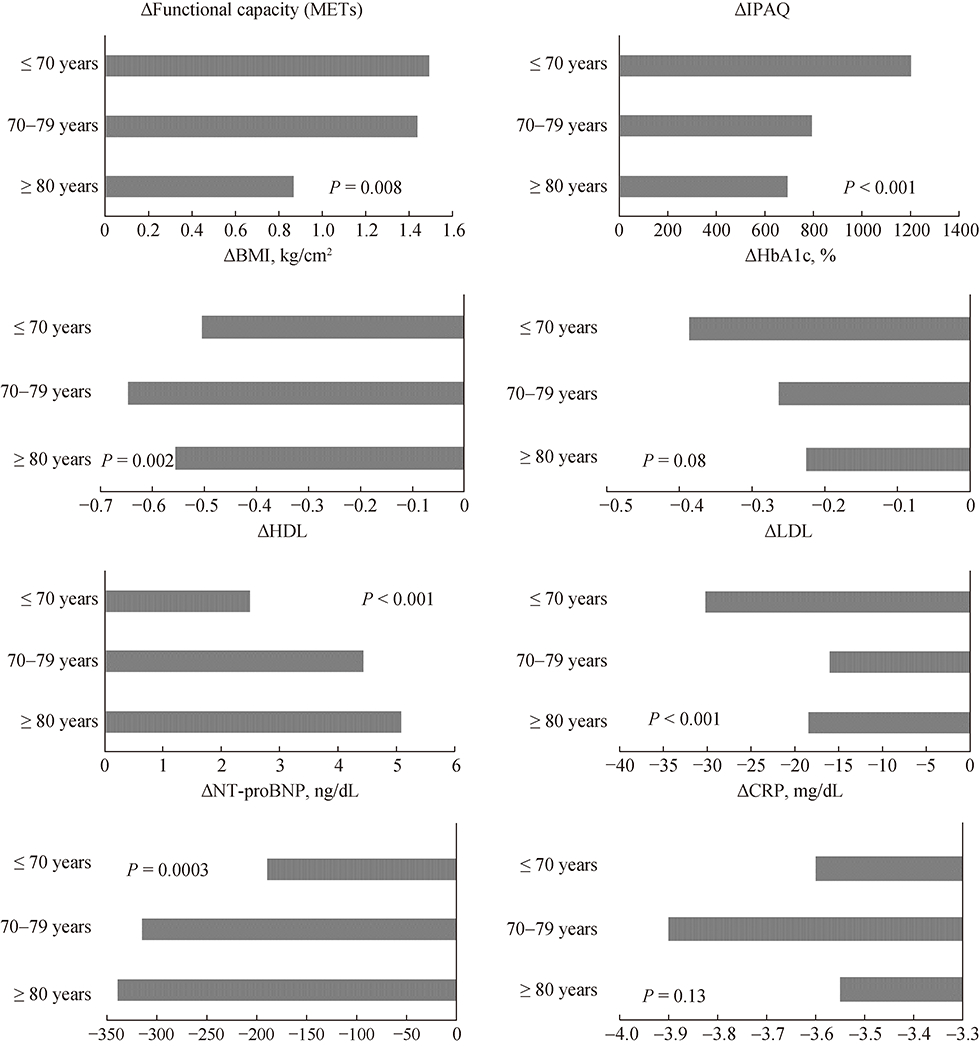
Both age groups showed similar improvements after the EBCR program (Table 2). Figure 1 illustrates the magnitude of the difference of multiple parameters between baseline and the end of phase Ⅱ EBCR evaluation across different age groups. Patients aged ≥ 70 years showed a smaller increased in functional capacity and physical activity measured by IPAQ score when compared to their younger counterparts. Patients aged between 60 and 79 years old showed the largest reduction in body mass index and abdominal perimeter. Regarding lipid profile, younger patients had a greater improvement in LDL-C, TG and HDL-C after EBCR. Older patients showed a larger reduction in NT pro-BNP between before and after supervised program, which was highest in the ≥ 80 years group. This dependence on age was not confirmed when using linear regression analysis with age as a continuous variable (Table 3). Using multivariate analysis with age as a continuous variable, adjusting for baseline differences between young and older patients (Table 1), only changes in IPAQ score and HbA1c were dependent on age.
| Univariate analysis | Multivariate analysis | ||||
| B coefficient | CI | B coefficient | CI | ||
| ΔFunctional capacity (METs) | 0.003 | -0.002-0.01 | 0.01 | -0.0005-0.02 | |
| ΔIPAQ | -0.02 | -0.007--0.02 | -0.01 | -0.02--0.01 * | |
| ΔBMI, Kg/m2 | 0.006 | -0.22-0.9 | 0.001 | -0.01-0.01 | |
| ΔAbdominal perimeter, cm | -0.006 | -0.03-0.02 | 0.02 | -0.02-0.06 | |
| ΔTotal cholesterol, mg/dL | 1.00 | 0.78-1.20 | 0.81 | -0.13-1.74 | |
| ΔHDL-C, mg/dL | 0.002 | -0.05-0.05 | 0.02 | -0.08-0.13 | |
| ΔLDL-C, mg/dL | 0.82 | 0.65-1.00 | 0.25 | -0.03-0.54 | |
| ΔTriglycerides, mg/dL | 0.86 | 0.48-1.24 | 0.07 | -0.61-0.47 | |
| ΔHbA1c, % | 0.006 | 0.001-0.01 | 0.01 | 0.002-0.02 * | |
| ΔNT-pro-BNP, ng/mL | 0.006 | -0.03-0.04 | 0.18 | -0.18-0.04 | |
| C reactive protein, mg/dL | -0.02 | -0.07-0.04 | -0.08 | -0.27-0.10 | |
| *Statistically significant. BMI: body mass index; CRP: cardiac rehabilitation program; HbA1c: glycated haemoglobin; HDL-C: high-density lipoprotein cholesterol; IPAQ: International Physical Activity Questionnaire; LDL-C: low-density lipoprotein cholesterol; METs: metabolic equivalents; NT-pro-BNP: NT pro-brain natriuretic peptide; TC: total cholesterol; TG: triglycerides. | |||||
This study of post-AMI patients who completed an EBCR program had the following major findings. First, patients had significant improvements on functional capacity, daily physical activity, metabolic profile, NT pro-BNP and inflammation, irrespective of age. Second, the magnitude of the beneficial effect of EBCR on most parameters was similar across age spectrum. Third, older patients showed a smaller benefit on the increment of physical activity measured by the IPAQ score and on the HbA1c reduction.
Older patients had more comorbidities than their younger counterparts. Their heart disease was also more severe, presenting with multivessel CAD more frequently and having higher NT-pro-BNP. This frailty of the older patients is frequently translated into longer hospital stays and higher rates of physical impairment after a cardiac event.[15] Also, older patients were taking more diuretics, calcium channel blockers and nitrates than younger patients.
Although the prevalence of cardiovascular events increases with age, in our sample only 21% of the patients were 70 years of age or older. This could be explained by the lower EBCR referral rates among the older patients, as previously reported in other studies.[31, 32] Older patients have higher rates of social isolation.[33] In our cohort, fewer older patients lived with their partner and more frequently were widowed. Social isolation and lack of social support in the older patients can contribute to lower adherence rates to secondary prevention strategies and have been shown to predict increased morbidity and mortality after an acute myocardial infarction.[34]
Patients aged ≥ 70 years achieved favourable outcomes in most of the studied parameters, regardless of their higher burden of comorbidities. These findings stress the need for strategies to increase the referral rate among these age groups.
Older patients had a better lipid profile than the young at the baseline. The magnitude of the improvement on LDL-C cholesterol and TG during EBCR was inferior in older patients, but this difference was not observed after adjusting for their baseline values. Al Quait, et al.[35] also demonstrated a difference of 30% on the reduction of total cholesterol after EBCR between older and younger patients, favouring the younger cohort. We found no significant differences on the percentage of patients taking statins between groups at the baseline, however we did not assess the prescribed dose of the statin, neither the discontinuation rate of this drug, which could influence outcomes.
Older patients had a more pronounced reduction of NT pro-BNP values during EBCR, which seems to be explained by their higher baseline value, since this difference lost significance when adjusted for baseline covariates. Previous studies have demonstrated similar reductions on this prognostic marker during EBCR.[17]
The role of functional capacity as an independent predictor of mortality has been established.[36, 37] In our cohort, older patients had a worse baseline functional capacity, evaluated by metabolic equivalents on a stress treadmill test. Ageing is usually associated with a gradual loss of muscle mass and a deterioration of oxygen uptake, which can explain these differences in addition to the impact of their high burden of comorbidities. Due to their low baseline exercise capacity, older patients may demonstrate larger improvements on cardiorespiratory fitness after EBCR.[38, 39] These findings are not consistent and Sandercock et al. showed significantly larger gains in cardiovascular fitness in patients with < 55 years old compared to their older counterparts.[40] In our cohort, young and older patients had similar improvements on functional capacity, with the exception of patients with ≥ 80 years of age, who showed smaller improvements on this outcome. Regarding daily physical activity measured by the IPAQ score, the youngest age group demonstrated larger gains after EBCR. Despite small differences on magnitude, this positive trend in both age groups supports the positive impact of EBCR on prognosis of patients after an acute myocardial infarction.
Finally, we find a consistent decrease of C reactive protein after EBCR in both age groups. This supports the hypothesis that exercise physical activity and exercise training contribute to decrease inflammation regardless of heart disease and age.[41] Despite the known association between aging and inflammation, [42] we did not find a statistically significant difference on reactive C protein between both age groups.
It is important to note that the observed improvements could also be explained by other factors than the EBCR. Regarding functional capacity, daily physical activity, reactive C protein and pro-BNP, it could be hypothesised that the since the first measurements were done after a hospitalization for AMI, the values were worse (more extreme) that the expected for those individuals. In such case, the regression to the mean phenomena could have contributed to the observed improvements. Moreover, after an acute myocardial infarction, patients are prone to adhere to lifestyle changes (like eating healthier food and doing exercise). They are also on medication like statins that were titrated according to the target values for each patient at their physician's description. These factors certainly contributed to the observed improvements. However, it is expected that at least in some degree the changes in these outcomes were affected by the EBCR itself, as demonstrated by several examples on the literature, including randomized clinical trials which compared patients who underwent CRP with controls who did not.[2]
Although cardiac rehabilitation is a major secondary prevention strategy and is currently indicated after an AMI as a class I level A recommendation, [5] older patients do not receive any specific mention on the guidelines. Future research should focus on the reasons of the lower referral rates of this specific population to EBCR, and strategies to counteract this tendency. Social and quality-of-life related outcomes on older patients should also be addressed in further studies.
Our study has several limitations. The number of EBCR sessions and the number of group education sessions attended by each patient was not available. It is plausible that this information could influence the results. Physicians tend to refer to EBCR older patients who have less comorbidities, greater functional capacity and who are more adherent to treatments. Also, about 19% of the patients were lost to follow up after initiating the EBCR program. Therefore, there is probably some degree of selection bias in our sample. With the large evidence available nowadays, it would not be ethically acceptable to deny EBCR to some patients. We did not assess major cardiovascular events in this study—it would not be reasonable to compare major events in older versus young patients, since these events are related with age, a confounder difficult to adjust for. Since the EBCR program occurred after an AMI, most patients have started medications or had their drugs adjusted during this period and were probably more motivated to adhere to lifestyle changes. This probably happened both in young and older patients and certainly accounted to some degree of the improvements that were observed, regardless of the impact of EBCR. We did not study the social and psychological impact of cardiac rehabilitation. Finally, in this study we only assessed the short-term impact of EBCR.
Both younger and older patients have significant improvements of functional capacity, metabolic profile and inflammation after the completion of an EBCR program. Although some differences exist on the degree of beneficial effect of EBCR between both groups, these variations are modest and both groups seem to benefit from EBCR at short-term. EBCR is a major secondary prevention strategy with recognized benefits and older patients should be systematically referred to it.
The authors received no financial support for the research, authorship, and/or publication of this article and have no disclosures to declare.
MFO, MT, SM, MS, SC and ST contributed to the conception of the study. MFO, MT and PF contributed to data collection. MFO and MS participated in statistical analysis. MFO drafted the manuscript. All authors critically revised the manuscript, gave final approval and agreed to be accountable for all aspects of work.
| [1] |
Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016; 37: 2315–2381. doi: 10.1093/eurheartj/ehw106
|
| [2] |
Anderson L, Oldridge N, Thompson DR, et al. Exercise-based cardiac rehabilitation for coronary heart disease: cochrane systematic review and meta-analysis. J Am Coll Cardiol 2016; 67: 1–12. https://pubmed.ncbi.nlm.nih.gov/26764059/
|
| [3] |
Lawler PR, Filion KB, Eisenberg MJ. Efficacy of exercise- based cardiac rehabilitation post-myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Am Heart J 2011; 162: 571–584.e2. doi: 10.1016/j.ahj.2011.07.017
|
| [4] |
Salzwedel A, Jensen K, Rauch B, et al. Effectiveness of comprehensive cardiac rehabilitation in coronary artery disease patients treated according to contemporary evidence based medicine: Update of the Cardiac Rehabilitation Outcome Study (CROS-Ⅱ). Eur J Prev Cardiol 2020; 2047487320905719. doi: 10.1177/2047487320905719
|
| [5] |
Ibanez B, James S, Agewall S, Antunes MJ, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018; 39: 119–177. doi: 10.1093/eurheartj/ehx393
|
| [6] |
Smith SC, Benjamin EJ, Bonow RO, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients With Coronary and Other Atherosclerotic Vascular Disease: 2011 Update: A Guideline From the American Heart Association and American College of Cardiology Foundation Endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol 2011; 58: 2432–2446. doi: 10.1016/j.jacc.2011.10.824
|
| [7] |
Yeh RW, Sidney S, Chandra M, et al. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med 2010; 362: 2155–2165. doi: 10.1056/NEJMoa0908610
|
| [8] |
Bourgeois FT, Orenstein L, Ballakur S, et al. Exclusion of elderly persons in randomized clinical trials of drugs for ischemic heart disease. J Am Geriatr Soc 2017; 65: 2354–2361. doi: 10.1111/jgs.14833
|
| [9] |
Devlin G. Women and elderly: subgroups under-represented in clinical trials. Curr Opin Cardiol 2010; 25: 335–339. doi: 10.1097/HCO.0b013e328338bcab
|
| [10] |
Anderson L, Thompson DR, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2016; CD001800. http://europepmc.org/abstract/MED/21735386
|
| [11] |
Dusseldorp E, van Elderen T, Maes S, Meulman J, Kraaij V. A meta-analysis of psychoeduational programs for coronary heart disease patients. Health Psychol 1999; 18: 506–519. doi: 10.1037/0278-6133.18.5.506
|
| [12] |
Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med 2004; 116: 682–692. doi: 10.1016/j.amjmed.2004.01.009
|
| [13] |
McConnell TR, Laubach CA, Memon M, et al. Quality of life and self efficacy in cardiac rehabilitation patients over 70 years of age following acute myocardial infarction and bypass revascularization surgery. Am J Geriatr Cardiol 2000; 9: 210–218. doi: 10.1111/j.1076-7460.2000.80040.x
|
| [14] |
Ades PA, Waldmann ML, Meyer WL, et al. Skeletal muscle and cardiovascular adaptations to exercise conditioning in older coronary patients. Circulation 1996; 94: 323–330. doi: 10.1161/01.CIR.94.3.323
|
| [15] |
Audelin MC, Savage PD, Ades PA. Exercise-based cardiac rehabilitation for very old patients (> or =75 years): focus on physical function. J Cardiopulm Rehabil Prev 2008; 28: 163–173. doi: 10.1097/01.HCR.0000320066.58599.e5
|
| [16] |
Listerman J, Bittner V, Sanderson BK, Brown TM. Cardiac rehabilitation outcomes: impact of comorbidities and age. J Cardiopulm Rehabil Prev 2011; 31: 342–348. doi: 10.1097/HCR.0b013e31822f189c
|
| [17] |
Rodrigues P, Santos M, Sousa MJ, et al. Cardiac rehabilitation after an acute coronary syndrome: the impact in elderly patients. Cardiology 2015; 131: 177–185. doi: 10.1159/000381824
|
| [18] |
Suaya JA, Stason WB, Ades PA, et al. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol 2009; 54: 25–33. doi: 10.1016/j.jacc.2009.01.078
|
| [19] |
Pasquali SK, Alexander KP, Peterson ED. Cardiac rehabilitation in the elderly. Am Heart J 2001; 142: 748–755. doi: 10.1067/mhj.2001.119134
|
| [20] |
Cortés O, Arthur HM. Determinants of referral to cardiac rehabilitation programs in patients with coronary artery disease: a systematic review. Am Heart J 2006; 151: 249–256. doi: 10.1016/j.ahj.2005.03.034
|
| [21] |
Ades PA, Waldmann ML, McCann WJ, Weaver SO. Predictors of cardiac rehabilitation participation in older coronary patients. Arch Intern Med 1992; 152: 1033–1035. doi: 10.1001/archinte.1992.00400170113021
|
| [22] |
Kumar KR, Pina IL. Cardiac rehabilitation in older adults: new options. Clin Cardiol 2019; 43: 163–170. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=10.1161/CIR.0000000000000747
|
| [23] |
Piepoli MF, Corrà U, Adamopoulos S, et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: a policy statement from the cardiac rehabilitation section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur J Prev Cardiol 2014; 21: 664–681. doi: 10.1177/2047487312449597
|
| [24] |
Karvonen MJ, Kentala E, Mustala O. The effects of training on heart rate; a longitudinal study. Ann Med Exp Biol Fenn 1957; 35: 307–315. http://onlinelibrary.wiley.com/resolve/reference/PMED?id=13470504
|
| [25] |
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982; 14: 377–381. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=WK_LWW2017052520149418
|
| [26] |
Mezzani A, Hamm LF, Jones AM, et al. Aerobic exercise intensity assessment and prescription in cardiac rehabilitation: a joint position statement of the European Association for Cardiovascular Prevention and Rehabilitation, the American Association of Cardiovascular and Pulmonary Rehabilitation and the Canadian Association of Cardiac Rehabilitation. Eur J Prev Cardiol 2013; 20: 442–467. doi: 10.1177/2047487312460484
|
| [27] |
Kim Y, Park I, Kang M. Convergent validity of the international physical activity questionnaire (IPAQ): meta-analysis. Public Health Nutr 2013; 16: 440–452. doi: 10.1017/S1368980012002996
|
| [28] |
Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003; 35: 1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB
|
| [29] |
Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015; 28: 1–39.e14. doi: 10.1016/j.echo.2014.10.003
|
| [30] |
Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009; 150: 604–612. doi: 10.7326/0003-4819-150-9-200905050-00006
|
| [31] |
Johnson N, Fisher J, Nagle A, et al. Factors associated with referral to outpatient cardiac rehabilitation services. J Cardiopulm Rehabil 2004; 24: 165–170. doi: 10.1097/00008483-200405000-00005
|
| [32] |
Barber K, Stommel M, Kroll J, et al. Cardiac rehabilitation for community-based patients with myocardial infarction: factors predicting discharge recommendation and participation. J Clin Epidemiol 2001; 54: 1025–1030. doi: 10.1016/S0895-4356(01)00375-4
|
| [33] |
Hämmig O. Health risks associated with social isolation in general and in young, middle and old age. PLoS One 2019; e0219663. http://www.researchgate.net/publication/334554650_Health_risks_associated_with_social_isolation_in_general_and_in_young_middle_and_old_age
|
| [34] |
Krumholz HM, Butler J, Miller J, et al. Prognostic importance of emotional support for elderly patients hospitalized with heart failure. Circulation 1998; 97: 958–964. doi: 10.1161/01.CIR.97.10.958
|
| [35] |
Al Quait A, Doherty P. Does cardiac rehabilitation favour the young over the old? Open Heart 2016; 3: e000450. doi: 10.1136/openhrt-2016-000450
|
| [36] |
Gulati M, Pandey DK, Arnsdorf MF, et al. Exercise capacity and the risk of death in women: the St James Women Take Heart Project. Circulation 2003; 108: 1554–1559. doi: 10.1161/01.CIR.0000091080.57509.E9
|
| [37] |
Kokkinos P, Myers J, Kokkinos JP, et al. Exercise capacity and mortality in black and white men. Circulation 2008; 117: 614–622. doi: 10.1161/CIRCULATIONAHA.107.734764
|
| [38] |
Lavie CJ, Milani RV. Effects of cardiac rehabilitation programs on exercise capacity, coronary risk factors, behavioral characteristics, and quality of life in a large elderly cohort. Am J Cardiol 1995; 76: 177–179. doi: 10.1016/S0002-9149(99)80054-X
|
| [39] |
Marchionni N, Fattirolli F, Fumagalli S, et al. Improved exercise tolerance and quality of life with cardiac rehabilitation of older patients after myocardial infarction: results of a randomized, controlled trial. Circulation 2003; 107: 2201–2206. doi: 10.1161/01.CIR.0000066322.21016.4A
|
| [40] |
Sandercock G, Hurtado V, Cardoso F. Changes in cardiorespiratory fitness in cardiac rehabilitation patients: a meta-analysis. Int J Cardiol 2013; 167: 894–902. doi: 10.1016/j.ijcard.2011.11.068
|
| [41] |
Hammonds TL, Gathright EC, Goldstein CM, Penn MS, Hughes JW. Effects of exercise on C-reactive protein in healthy patients and in patients with heart disease: A meta-analysis. Heart Lung 2016; 45: 273–282. doi: 10.1016/j.hrtlng.2016.01.009
|
| [42] |
Milan-Mattos JC, Anibal FF, Perseguini NM, et al. Effects of natural aging and gender on pro-inflammatory markers. Braz J Med Biol Res 2019; 52: e8392. doi: 10.1590/1414-431x20198392
|
| [1] | Hee-Eun Choi, Chul Kim, Se-Heum Park, Doo-Il Kim, Ki-Hun Kim, Dong-Kie Kim, Seunghwan Kim, Jino Park. Polymorphic ventricular tachycardia during phase II cardiac rehabilitation in a patient with heart failure: a case report[J]. Journal of Geriatric Cardiology, 2020, 17(1): 64-66. DOI: 10.11909/j.issn.1671-5411.2020.01.003 |
| [2] | Cheng GE, Jing MA, Yong XU, Ya-Jun SHI, Cheng-Hui ZHAO, Ling GAO, Jing BAI, Yu WANG, Zhi-Jun SUN, Jun GUO, Yun-Dai CHEN. Predictors of adherence to home-based cardiac rehabilitation program among coronary artery disease outpatients in China[J]. Journal of Geriatric Cardiology, 2019, 16(10): 749-755. DOI: 10.11909/j.issn.1671-5411.2019.10.003 |
| [3] | Jia-Ying FANG, Ji-Lin LI, Zhong-Han LI, Duan-Min XU, Chang CHEN, Bin XIE, Helen CHEN, William W AU. Attitudes towards acceptance of an innovative home-based and remote sens-ing rehabilitation protocol among cardiovascular patients in Shantou, China[J]. Journal of Geriatric Cardiology, 2016, 13(4): 326-332. DOI: 10.11909/j.issn.1671-5411.2016.04.006 |
| [4] | Mauro Feola, Sonia Garnero, Beatrice Daniele, Claudia Mento, Fabio Dell’Aira, Giuliana Chizzolini, Marzia Testa. Gender differences in the efficacy of cardiovascular rehabilitation in patients after cardiac surgery procedures[J]. Journal of Geriatric Cardiology, 2015, 12(5): 575-579. DOI: 10.11909/j.issn.1671-5411.2015.05.015 |
| [5] | Seahyoung Lee, Eunhyun Choi, Min-Ji Cha, Ae-Jun Park, Cheesoon Yoon, Ki-Chul Hwang. Impact of miRNAs on cardiovascular aging[J]. Journal of Geriatric Cardiology, 2015, 12(5): 569-574. DOI: 10.11909/j.issn.1671-5411.2015.05.011 |
| [6] | Abdulla Damluji, Archana Ramireddy, Lynda Otalvaro, Daniel E Forman. Secondary cardiovascular prevention in older adults: an evidence based review[J]. Journal of Geriatric Cardiology, 2015, 12(5): 459-464. DOI: 10.11909/j.issn.1671-5411.2015.05.019 |
| [7] | Juan Pedro-Botet, Elisenda Climent, Juan J Chillarón, Rocio Toro, David Benaiges, Juana A Flores-Le Roux. Statins for primary cardiovascular prevention in the elderly[J]. Journal of Geriatric Cardiology, 2015, 12(4): 431-438. DOI: 10.11909/j.issn.1671-5411.2015.04.016 |
| [8] | Renzo Zanettini, Gemma Gatto, Ileana Mori, Maria Beatrice Pozzoni, Stefano Pelenghi, Luigi Martinelli, Silvio Klugmann. Cardiac rehabilitation and mid-term follow-up after transcatheter aortic valve implantation[J]. Journal of Geriatric Cardiology, 2014, 11(4): 279-285. DOI: 10.11909/j.issn.1671-5411.2014.04.001 |
| [9] | Simon W. Rabkin. Aging effects on QT interval: Implications for cardiac safety of antipsychotic drugs[J]. Journal of Geriatric Cardiology, 2014, 11(1): 20-25. DOI: 10.3969/j.issn.1671-5411.2014.01.005 |
| [10] | Arthur R Menezes, Carl J Lavie, Richard V Milani, Ross A Arena, Timothy S Church. Cardiac rehabilitation and exercise therapy in the elderly: Should we invest in the aged?[J]. Journal of Geriatric Cardiology, 2012, 9(1): 68-75. DOI: 10.3724/SP.J.1263.2012.00068 |
| All patients (n = 1607) | < 70 years old (n = 1274) | ≥ 70 years old (n = 333) | P-value | |
| Age, yrs | 60.4 ± 10.3 | 56.8 ± 8.1 | 74.3 ± 3.1 | < 0.001 |
| Gender, female | 19.4% | 18.5% | 22.8% | 0.08 |
| Hypertension | 57.0% | 52.8% | 73.0% | < 0.001 |
| Diabetes mellitus | 33.4% | 32.4% | 37.4% | 0.14 |
| Dyslipidemia | 68.9% | 68.5% | 70.2% | 0.56 |
| Smoking | ||||
| Current smoker | 38.7.7% | 44.8% | 16.2% | < 0.001 |
| Past smoker | 12.0% | 12.9% | 8.4% | |
| Obesity | 49.5% | 50.1% | 47.4% | 0.39 |
| BMI, kg/m2 | 26.3 ± 3.8 | 26.4 ± 3.9 | 25.8 ± 3.6 | 0.02 |
| Abdominal perimeter, cm | 97.2 ± 9.9 | 96.9 ± 9.9 | 98.0 ± 9.8 | 0.07 |
| Multivessel disease | 66.1% | 64.2% | 73.1% | 0.02 |
| 3-vessel disease | 34.1% | 32.8% | 39.2% | |
| STEMI | 35.8% | 39.0% | 26.1% | 0.11 |
| Moderate LVSD | 9.9% | 11.1% | 5.3% | 0.39 |
| Severe LVSD | 6.0% | 5.3% | 8.6% | |
| NT pro-BNP, ng/mL | 457 (210–1064) | 410 (190–901) | 838 (280–1722) | < 0.001 |
| Glomerular filtration rate, mL/min | 67.3 ± 27.1 | 70.4 ± 27.3 | 55.5 ± 23.3 | < 0.001 |
| Marital status | ||||
| Married/living with partner | 81.4% | 82.3% | 77.9% | |
| Single | 5.4% | 5.8% | 3.7% | < 0.001 |
| Divorced | 7.3% | 8.3% | 3.7% | |
| Widowed | 5.9% | 3.5% | 14.8% | |
| β-blockers | 81.6% | 84.6% | 70.2% | < 0.001 |
| ACEI or ARB | 62.6% | 61.3% | 67.8% | 0.06 |
| Statins | 95.9% | 96.5% | 93.9% | 0.07 |
| Diuretics | 17.3% | 15.3% | 24.9% | < 0.001 |
| Calcium channel blockers | 11.1% | 9.4% | 17.4% | 0.001 |
| Nitrates | 19.5% | 17.8% | 25.7% | 0.005 |
| Total cholesterol, mg/dL | 174.6 ± 41.2 | 177.4 ± 41.7 | 163.5 ± 37.1 | < 0.001 |
| HDL-C, mg/dL | 40.7 ± 11.7 | 40.4 ± 0.3 | 42.3 ± 0.6 | 0.008 |
| LDL-C, mg/dL | 105.8 ± 34.8 | 108.0 ± 35.2 | 97.1 ± 32.0 | < 0.001 |
| Triglycerides, mg/dL | 144.5 ± 85.2 | 149.7 ± 90.1 | 124.3 ± 58.1 | < 0.001 |
| HbA1c, % | 6.3 ± 1.3 | 6.3 ± 1.3 | 6.3 ± 1.0 | 0.32 |
| CRP, mg/dL | 5.7 (2.4-12.2) | 5.7 (2.5-12.2) | 5.3 (2.4-12.5) | 0.47 |
| Functional capacity (METs) | 8.6 ± 2.3 | 9.0 ± 2.3 | 7.0 ± 1.9 | < 0.001 |
| IPAQ | 0 (0-693) | 0 (0-693) | 0 (0-693) | 0.94 |
| Data are presented as mean ± SD or median (interquartile range) unless other indicated. ACEI: angiotensin-converting enzyme inhibitors; ARB: angiotensin receptor blockers; BMI: body mass index; CRP: C-reactive protein; HbA1c: glycated haemoglobin; HDL-C: high-density lipoprotein cholesterol; IPAQ: International Physical Activity Questionnaire; IQR: interquartile range; LDL-C: low-density lipoprotein cholesterol; LVSD: left ventricle systolic dysfunction; MET: metabolic equivalenttask; NT pro-BNP: NT pro-brain natriuretic peptide; STEMI: ST-segment elevation myocardial infarction. | ||||
| Characteristic | All patients (n = 1607) | < 70 years old (n = 1274) | ≥ 70 years old (n = 333) | |||||||||||
| Baseline | After EBCR | Delta Δ | P value | Baseline | After EBCR | Delta Δ | P value | Baseline | After EBCR | Delta Δ | P value | |||
| Functional capacity (METs) | 8.6 ± 2.3 | 10.0 ± 2.3 | 1.4 ± 1.2 | < 0.001 | 9.0 ± 2.3 | 10.4 ± 2.2 | 1.5 ± 1.2 | < 0.001 | 7.0 ± 1.9 | 8.4 ± 2.0 | 1.4 ± 1.2 | < 0.001 | ||
| IPAQ | 0 (0-693) | 1386 (990-2142) | 1094 (594-1533) | < 0.001 | 0 (0-693) | 1386 (1040-2384) | 1200 (693-1680) | < 0.001 | 0 (0-693) | 1386 (693-1434) | 693 (396-1386) | < 0.001 | ||
| BMI, kg/m2 | 26.3 ± 3.8 | 25.8 ± 3.7 | -0.6 ± 1.0 | < 0.001 | 26.4 ± 3.9 | 25.9 ± 3.8 | -0.5 ± 1.0 | < 0.001 | 25.8 ± 3.6 | 25.2 ± 3.5 | -0.6 ± 0.8 | < 0.001 | ||
| Abdominal perimeter, cm | 97.2 ± 9.9 | 94.4 ± 10.2 | -2.8 ± 5.8 | < 0.001 | 96.9 ± 9.9 | 94.2 ± 10.1 | -2.7 ± 5.6 | < 0.001 | 98.0 ± 9.8 | 95.1 ± 10.6 | -2.9 ± 6.5 | < 0.001 | ||
| Total cholesterol, mg/dL | 174.6 ± 41.1 | 147.6 ± 35.2 | -29.7 ± 42.1 | < 0.001 | 177.4 ± 41.7 | 147.3 ± 34.6 | -33.0 ± 42.8 | < 0.001 | 163.5 ± 37.1 | 148.7 ± 37.6 | -16.2 ± 36.0 | < 0.001 | ||
| HDL-C, mg/dL | 40.7 ± 11.7 | 44.4 ± 12.1 | 2.2 ± 9.1 | < 0.001 | 40.4 ± 0.3 | 43.1 ± 12.0 | 2.0 ± 9.2 | < 0.001 | 42.3 ± 0.6 | 46.8 ± 12.0 | 3.1 ± 8.1 | 0.001 | ||
| LDL-C, mg/dL | 105.8 ± 34.8 | 80.9 ± 28.5 | -27.4 ± 35.5 | < 0.001 | 108.0 ± 35.2 | 80.6 ± 27.6 | -30.2 ± 35.8 | < 0.001 | 97.1 ± 32.0 | 82.2 ± 31.7 | -16.3 ± 32.1 | 0.0001 | ||
| Triglycerides, mg/dL | 144.5 ± 85.2 | 117.8 ± 58.1 | -30.0 ± 75.5 | < 0.001 | 149.7 ± 90.1 | 120.2 ± 61.0 | -33.0 ± 80.2 | < 0.001 | 124.3 ± 58.1 | 108.2 ± 44.3 | -18.2 ± 51.4 | 0.0181 | ||
| HbA1c, % | 6.3 ± 1.3 | 6.0 ± 1.0 | -0.4 ± 0.8 | < 0.001 | 6.3 ± 1.3 | 6.0 ± 1.0 | -0.4 ± 0.8 | < 0.001 | 6.3 ± 1.0 | 6.1 ± 0.9 | -0.3 ± 0.6 | < 0.001 | ||
| NT pro-BNP, ng/mL | 457 (210-1064) | 242 (106-562) | -201 (514--41) | < 0.001 | 410 (190-901) | 217 (93-511) | -189 (451--38) | < 0.001 | 838 (280-1722) | 412 (190-1016) | -321 (-914--68) | < 0.001 | ||
| CRP, mg/dL | 5.7 (2.4-12.2) | 1.8 (0.9-3.4) | -3.7 (-9.6--0.7) | < 0.001 | 5.7 (2.5-12.2) | 1.8 (0.9-3.5) | -3.6 (-9.6--0.8) | < 0.001 | 5.3 (2.4-12.5) | 2.0 (1.2-3.1) | -3.9 (-9.8--0.6) | < 0.001 | ||
| Glomerular filtration rate, mL/min | 76.0 ± 42.6 | 65.6 ± 28.0 | -10.7 ± 28.1 | < 0.001 | 79.1 ± 43.7 | 68.4 ± 28.7 | -11.0 ± 29.0 | < 0.001 | 63.8 ± 35.5 | 54.6 ± 21.4 | -9.3 ± 24.5 | < 0.001 | ||
| Current smokers, % | 38.7 | 13.3 | -25.4 | < 0.001 | 44.8 | 14.3 | -30.5 | < 0.001 | 16.2 | 9.6 | -6.6 | < 0.001 | ||
| Cigarettes / day, n* | 20 (10-30) | 5 (3-10) | -9 (19-0) | < 0.001 | 20 (10-30) | 5 (3-10) | -9 (19-0) | < 0.001 | 20 (15-35) | 7 (4-8) | -4 (-18--2) | < 0.001 | ||
| Data are presented as mean ± SD or median (interquartile range) unless other indicated. BMI: body mass index; CRP: C-reactive protein; EBCR: exercise-based cardiac rehabilitation; HbA1c: glycated haemoglobin; HDL-C: high-density lipoprotein cholesterol; IPAQ: International Physical Activity Questionnaire; LDL-C: low-density lipoprotein cholesterol; METs: metabolic equivalents; NT-pro-BNP: NT pro-brain natriuretic peptide; *Cigarettes/day from patients who continued to smoke after EBCR. | ||||||||||||||
| Univariate analysis | Multivariate analysis | ||||
| B coefficient | CI | B coefficient | CI | ||
| ΔFunctional capacity (METs) | 0.003 | -0.002-0.01 | 0.01 | -0.0005-0.02 | |
| ΔIPAQ | -0.02 | -0.007--0.02 | -0.01 | -0.02--0.01 * | |
| ΔBMI, Kg/m2 | 0.006 | -0.22-0.9 | 0.001 | -0.01-0.01 | |
| ΔAbdominal perimeter, cm | -0.006 | -0.03-0.02 | 0.02 | -0.02-0.06 | |
| ΔTotal cholesterol, mg/dL | 1.00 | 0.78-1.20 | 0.81 | -0.13-1.74 | |
| ΔHDL-C, mg/dL | 0.002 | -0.05-0.05 | 0.02 | -0.08-0.13 | |
| ΔLDL-C, mg/dL | 0.82 | 0.65-1.00 | 0.25 | -0.03-0.54 | |
| ΔTriglycerides, mg/dL | 0.86 | 0.48-1.24 | 0.07 | -0.61-0.47 | |
| ΔHbA1c, % | 0.006 | 0.001-0.01 | 0.01 | 0.002-0.02 * | |
| ΔNT-pro-BNP, ng/mL | 0.006 | -0.03-0.04 | 0.18 | -0.18-0.04 | |
| C reactive protein, mg/dL | -0.02 | -0.07-0.04 | -0.08 | -0.27-0.10 | |
| *Statistically significant. BMI: body mass index; CRP: cardiac rehabilitation program; HbA1c: glycated haemoglobin; HDL-C: high-density lipoprotein cholesterol; IPAQ: International Physical Activity Questionnaire; LDL-C: low-density lipoprotein cholesterol; METs: metabolic equivalents; NT-pro-BNP: NT pro-brain natriuretic peptide; TC: total cholesterol; TG: triglycerides. | |||||