| Citation: | Please cite this article as: Ponzoni M, Fiocco A, Caraffa R, Nadali M, Longinotti L, Pradegan N, Bifulco O, Besola L, Fovino LN, Tarantini G, Colli A, Gerosa G. Institutional re-evolution of mitral valve procedures. J Geriatr Cardiol 2022; 19(7): 551−554. DOI: 10.11909/j.issn.1671-5411.2022.07.002. |
The introduction of transcatheter aortic valve replacement changed our approach for those patients with a high-to-prohibitive risk profile, and, more recently, for those with an intermediate-to-low risk profile.[1] Similarly, patients with mitral valve regurgitation (MVR) can now benefit from various transcatheter technologies, whose indications and recommendations are the subject of intense clinical investigation.[2]
Undetected valvular heart diseases may affect 50% of subjects in the elderly population, with an estimated prevalence that is expected to double before 2050.[3] In this scenario, patients affected by MVR may present a high surgical risk, that frequently contraindicates conventional surgery.[4] For this reason, transcatheter mitral valve technologies (TMVT) have been suggested by the most recent ESC/EACTS guidelines as safe alternatives in patients with contraindications for surgery or prohibitive operative risk.[2] Based on good safety and efficacy profiles, TMVT include edge-to-edge repair, chordal implantation, direct and indirect annuloplasty, and mitral valve replacement devices.[5] This broad transcatheter “mitral toolbox” provides the opportunity to treat every component of the mitral apparatus, offering a real “patient-tailored” approach, and potentially expanding treatment indications to a wider spectrum of individuals.[6] We aimed to analyze the impact of the introduction of TMVT on patients’ referral and early outcomes at our institution.
We retrospectively reviewed all consecutive patients with severe MVR (both functional and degenerative forms) treated at our institution between January 2009 and December 2018. Patients referred in the last years were excluded due to the surgical activity modification consequent to the COVID-19 pandemic. The study was approved by the institutional Ethics Committee (Sep. 2021). Patients were divided into two “periods” according to the systematic adoption of TMVT from January 2014: Surgery-Only-Period (Jan. 2009-Dec. 2013) and Surgery-TMVT-Mixed-Period (Jan. 2014-Dec 2018). The number of MVR procedures was indexed to the total surgery volume (TSV) of both periods, thus removing a biasing effect of a different TSV.
Patients in the Surgery-TMVT-Mixed-Period were assigned to specific treatments based on a Heart Team discussion. Early outcomes (in-hospital or 30-days) were defined according to MVARC criteria. Descriptive statistic was used to summarize data. Quantitative variables were compared across surgical eras with the independent t-test and categorical variables with the chi-square test, as appropriate. Analyses were performed using SPSS 23.0 (IBM Corporation, Armonk, NY).
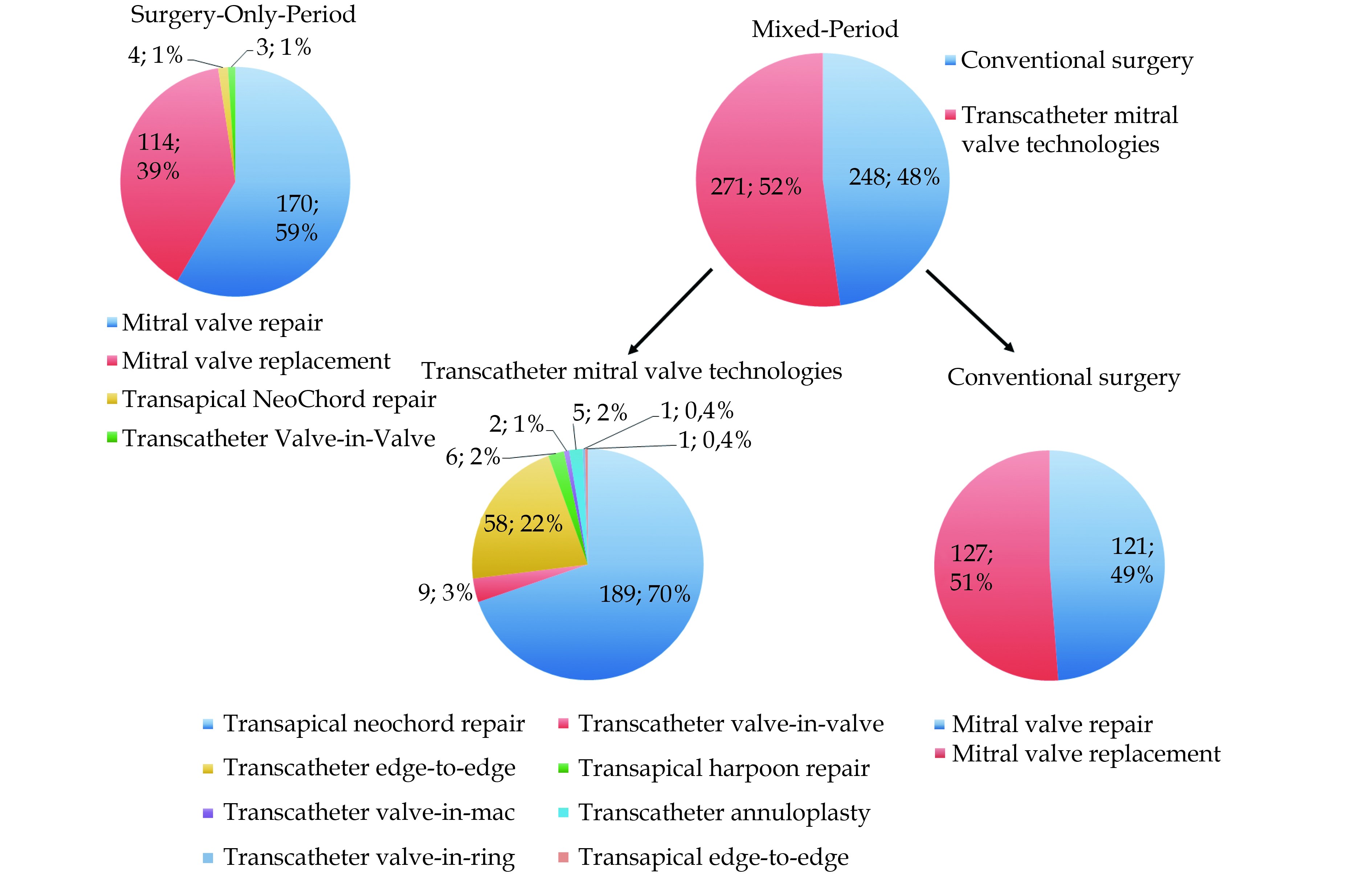
In the Surgery-Only-Period, 291 patients were referred to our center for MVR (9.1% of TSV): 170 patients (58.4%) underwent mitral valve repair, 119 (39.2%) mitral valve replacement, 4 (1.4%) transapical NeoChord repair, and 3 (1.0%) transcatheter mitral valve-in-valve replacement (Figure S1). In the Surgery-TMVT-Mixed-Period, 519 patients were referred to our center (14.1% of TSV): 248 (47.8%) patients underwent conventional surgery, while 271 (52.2%) were treated with TMVT (6.7% and 7.4% of TSV, respectively). Among the 248 conventional operations, 127 (51.2%) were mitral valve replacements and 121 (48.8%) were mitral valve repairs. Conversely, among the 271 TMVT procedures, 189 (69.7%) were transapical NeoChord repairs, 58 (21.4%) were edge-to-edge procedures, 9 (3.3%) were mitral valve-in-valve procedures, 6 (2.2%) were transapical chordal Harpoon repairs, 5 (1.9%) were transcatheter annuloplasties, 2 (0.7%) were valve-in-MAC, 1 (0.4%) was a valve-in-ring, and 1 (0.4%) was a transapical edge-to-edge (Figure 1). Table 1 summarizes baseline characteristics and early postoperative outcomes of patients.
| Surgery-Only-Period (n = 291) | Surgery-TMVT-Mixed-Period | |||
| Conventional surgery (n = 248) | TMVT (n = 271) | Overall (n = 519) | ||
| Baseline characteristics | ||||
| Age, yrs | 65.9 ± 12.6 | 68.1 ± 11.7* | 65.5 ± 12.9 | 66.8 ± 12.4 |
| EuroSCORE-II, % | 2.4 ± 3.3 | 2.4 ± 2.6 | 3.3 ± 5.7* | 2.9 ± 4.5 |
| Ejection fraction, % | 60.5 ± 10.3 | 59.6 ± 11.4 | 62.2 ± 8.3 | 61.1 ± 9.8 |
| Left-ventricular EDVI, mL/m² | 82.2 ± 21.7 | 82.6 ± 26.4 | 81.7 ± 20.9 | 82.1 ± 23.3 |
| PASP, mmHg | 41.7 ± 16.1 | 46.1 ± 17 | 38 ± 13.9 | 39.9 ± 15.1 |
| Male | 182 (62.6%) | 165 (66.5%) | 204 (75.3%)* | 369 (71.1%)* |
| NYHA class ≥ 3 | 108 (37.1%) | 86 (34.7%) | 133 (49.1%)* | 219 (42.2%)* |
| Reinterventions | 31 (10.7%) | 36 (14.5%) | 36 (13.3%) | 72 (13.9%) |
| Degenerative MVR | 246 (84.5%) | 210 (84.7%) | 231 (85.2%) | 441 (85%) |
| Functional MVR | 45 (15.5%) | 38 (15.3%) | 40 (14.8%) | 78 (15%) |
| Early Outcomes | ||||
| ICU stay, days | 1.9 ± 2.3 | 3.4 ± 7.8* | 1.5 ± 1.6* | 2.4 ± 5.6) |
| Total hospital stay, days | 10.6 ± 6.3 | 13.5 ± 17.8* | 10.2 ± 9.9 | 11.8 ± 14.2) |
| Ejection fraction, % | 54.7 ± 10.3 | 52.1 ± 9.1* | 50.5 ± 12.3* | 51.2 ± 11* |
| Left-ventricular EDVI, mL/m² | 66.5 ± 20.6 | 65.3 ± 20.1 | 78.4 ± 28.5* | 71.9 ± 25.5* |
| Residual MVR > moderate | 8 (2.7%) | 5 (2%) | 26 (9.6%)* | 31 (6%)* |
| Technical success | 286 (98.3%) | 247 (99.6%) | 262 (96.7%) | 509 (98.1%) |
| Device success | 284 (97.6%) | 246 (99.2%) | 258 (95.2%) | 504 (97.1%) |
| Procedure success | 283 (97.3%) | 238 (96%) | 253 (93.4%)* | 491 (94.6%) |
| All-cause death | 1 (0.4%) | 4 (1.6%) | 6 (2.2%) | 10 (1.9%) |
| Cardiovascular death | 1 (0.4%) | 4 (1.6%) | 5 (1.9%) | 9 (1.7%) |
| Stroke | 12 (4.1%) | 9 (3.6%) | 4 (1.5%) | 13 (2.5%) |
| Acute myocardial infarction | 1 (0.4%) | 0 | 1 (0.4%) | 1 (0.2%) |
| Reintervention Rate | 8 (2.7%) | 10 (4%)* | 7 (2.6%) | 17 (3.3%)* |
| Data are presented as mean ± SD or n (%). *P < 0.05 at independent t-test between the two periods. EDVI: end-diastolic volume-index; ICU: intensive care unit; MVR: mitral valve regurgitation; PASP: pulmonary artery systolic pressure; SD: standard deviation; TMVT: transcatheter-mitral-valve-technologies. | ||||
After the systematic adoption of TMVT, we observed a 54.1% increase in patients’ referral at our institution (9.1% vs. 14.1%; P < 0.001). In a 5-year period, TMVT presented a dramatic escalation from 0.2% to 7.4% of TSV (+3244.8%, P < 0.001), while conventional surgery reduced from 8.9% to 6.7% of TSV (-25%, P < 0.001). These findings suggest that a quote of patients who were previously considered for conventional surgery is currently scheduled for TMVT and that the absolute number of referred patients increased.
The introduction of transcatheter devices also modified the treatment indications for a significant quote of patients (Figure 2). Isolated MVR showed an 11.7% increase within total mitral valve interventions between the two periods (71.8% vs. 80.2%; P = 0.007) and a concomitant 18.2% decrease within conventional mitral surgery (71.8% vs. 58.5%; P < 0.001). While the approach for referred patients with combined diseases involving coronary arteries and/or other valves remained stable between the two periods. This confirms our previous findings, proving that the adoption of TMVT expanded the number of treated patients both increasing the total number of patients referred for isolated MVR, and increasing the number of patients with a prohibitive surgical risk.
In fact, we registered an increase in patients’ age, operative risk (EuroSCORE-II), and NYHA-class at admission across the two eras (Table 1). Conversely, procedure failure and residual >moderate regurgitation were more frequent in the Surgery-TMVT-Mixed-Period because successfully performing TMVT requires a learning curve and the acquisition of new procedural and imaging skills.[7]
Despite a more challenging population and a learning curve for TMVT, early mortality remained stable between periods (0.4% vs. 2%, P > 0.05), with a one-third incidence of stroke for TMVT (4.2% vs. 1.5%, P = 0.074) than the earlier era, confirming the relative safeness of the adoption of TMVT in a previously purely conventional surgical center.
In conclusion, the introduction of TMVT into our clinical practice not only increased the number of referred patients but allowed a safe treatment of a more complex and frail population. We confirm the importance of offering a wide spectrum of treatment options that provide real-world, patient-tailored strategies for MVR, especially in the elderly population.
| [1] |
Ueshima D, Fovino LN, D’Amico G, et al. Transcatheter versus surgical aortic valve replacement in low- and intermediate-risk patients: an updated systematic review and meta-analysis. Cardiovasc Interv Ther 2019; 34: 216−225. doi: 10.1007/s12928-018-0546-5
|
| [2] |
Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2022; 43: 561−632. doi: 10.1093/eurheartj/ehab395
|
| [3] |
d’Arcy JL, Coffey S, Loudon MA, et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: the OxVALVE Population Cohort Study. Eur Heart J 2016; 37: 3515−3122. doi: 10.1093/eurheartj/ehw229
|
| [4] |
Zhuge RQ, Hou XP, Qi XL, et al. Clinical features and treatment options for mitral regurgitation in elderly inpatients. J Geriatr Cardiol 2018; 15: 428−433.
|
| [5] |
Gupta T, Khera S, Kolte D, et al. Trends in Utilization of Surgical and Transcatheter Mitral Valve Repair in the United States. Am J Cardiol 2019; 123: 1187−1189. doi: 10.1016/j.amjcard.2019.01.005
|
| [6] |
Cepas-Guillén PL, Pascual I, Garcia E, et al. Transcatheter mitral valve repair in nonagenarians. J Geriatr Cardiol 2022; 19: 90−94.
|
| [7] |
Colli A, Bagozzi L, Banchelli F, et al. Learning curve analysis of transapical NeoChord mitral valve repair. Eur J Cardiothorac Surg 2018; 54: 273−280. doi: 10.1093/ejcts/ezy046
|
| [1] | Shishir Gupta, Sohum Sheth, Sujay Kamisetty, Marco Foreman, David Winchester. Cardiovascular outcomes and mortality after abnormal myocardial perfusion scans in the elderly: a re study at a tertiary care institution[J]. Journal of Geriatric Cardiology, 2023, 20(10): 760-761. DOI: 10.26599/1671-5411.2023.10.008 |
| [2] | Sebastian Alejandro Mikulic, José Ramón Rivas, Hui-Jun GUO, Khadeeja Esmail. The misfit mitral valve[J]. Journal of Geriatric Cardiology, 2021, 18(10): 855-856. DOI: 10.11909/j.issn.1671-5411.2021.10.008 |
| [3] | Jia-You TANG, Yang LIU, Jian YANG. A novel case of transcatheter mitral valve-in-valve replacement using Mi-thosTM system[J]. Journal of Geriatric Cardiology, 2020, 17(4): 229-233. DOI: 10.11909/j.issn.1671-5411.2020.04.007 |
| [4] | Pujan Patel, Shreya Ghetiya, Emil Missov, Srinivasan Sattiraju. A 3-dimensional transoesophageal echocardiography perspective of mitral valve abscess[J]. Journal of Geriatric Cardiology, 2020, 17(2): 124-124. DOI: 10.11909/j.issn.1671-5411.2020.02.009 |
| [5] | Gabriela S Gheorghe, Ana Ciobanu, Ioan T Nanea, Andreea S Şerban, Mihaela R Mititelu. Particular evolution in a 72-year-old diabetic patient with acute coronary syndrome[J]. Journal of Geriatric Cardiology, 2018, 15(7): 513-516. DOI: 10.11909/j.issn.1671-5411.2018.07.008 |
| [6] | Rui-Qi ZHUGE, Xiao-Pei HOU, Xi-Ling QI, Yong-Jian WU, Ming-Zi ZHANG. Clinical features and treatment options for mitral regurgitation in elderly inpatients[J]. Journal of Geriatric Cardiology, 2018, 15(6): 428-433. DOI: 10.11909/j.issn.1671-5411.2018.06.005 |
| [7] | Konstantinos C Theodoropoulos, Giovanni Masoero, Gianpiero Pagnano, Nicola Walker, Alexandros Papachristidis, Mark J Monaghan. Mitral pseudostenosis due to a large left atrial myxoma[J]. Journal of Geriatric Cardiology, 2018, 15(3): 244-245. DOI: 10.11909/j.issn.1671-5411.2018.03.009 |
| [8] | Aamir Shamsi, Mohammed Shah, Sudhir Rathore. Transradial approach for coronary procedures in the elderly population[J]. Journal of Geriatric Cardiology, 2016, 13(9): 798-806. DOI: 10.11909/j.issn.1671-5411.2016.09.002 |
| [9] | Ho-Ping Yu, Chi-Hung Huang, Shaw-Min Hou, Ming-Chon Hsiung, Shen-Kou Tsai, Wei-Hsian Yin. Percutaneous transcatheter closure of mitral paravalvular leak via transarterial retrograde approach[J]. Journal of Geriatric Cardiology, 2015, 12(6): 683-686. DOI: 10.11909/j.issn.1671-5411.2015.06.008 |
| [10] | Mauro Feola, Sonia Garnero, Beatrice Daniele, Claudia Mento, Fabio Dell’Aira, Giuliana Chizzolini, Marzia Testa. Gender differences in the efficacy of cardiovascular rehabilitation in patients after cardiac surgery procedures[J]. Journal of Geriatric Cardiology, 2015, 12(5): 575-579. DOI: 10.11909/j.issn.1671-5411.2015.05.015 |
| Surgery-Only-Period (n = 291) | Surgery-TMVT-Mixed-Period | |||
| Conventional surgery (n = 248) | TMVT (n = 271) | Overall (n = 519) | ||
| Baseline characteristics | ||||
| Age, yrs | 65.9 ± 12.6 | 68.1 ± 11.7* | 65.5 ± 12.9 | 66.8 ± 12.4 |
| EuroSCORE-II, % | 2.4 ± 3.3 | 2.4 ± 2.6 | 3.3 ± 5.7* | 2.9 ± 4.5 |
| Ejection fraction, % | 60.5 ± 10.3 | 59.6 ± 11.4 | 62.2 ± 8.3 | 61.1 ± 9.8 |
| Left-ventricular EDVI, mL/m² | 82.2 ± 21.7 | 82.6 ± 26.4 | 81.7 ± 20.9 | 82.1 ± 23.3 |
| PASP, mmHg | 41.7 ± 16.1 | 46.1 ± 17 | 38 ± 13.9 | 39.9 ± 15.1 |
| Male | 182 (62.6%) | 165 (66.5%) | 204 (75.3%)* | 369 (71.1%)* |
| NYHA class ≥ 3 | 108 (37.1%) | 86 (34.7%) | 133 (49.1%)* | 219 (42.2%)* |
| Reinterventions | 31 (10.7%) | 36 (14.5%) | 36 (13.3%) | 72 (13.9%) |
| Degenerative MVR | 246 (84.5%) | 210 (84.7%) | 231 (85.2%) | 441 (85%) |
| Functional MVR | 45 (15.5%) | 38 (15.3%) | 40 (14.8%) | 78 (15%) |
| Early Outcomes | ||||
| ICU stay, days | 1.9 ± 2.3 | 3.4 ± 7.8* | 1.5 ± 1.6* | 2.4 ± 5.6) |
| Total hospital stay, days | 10.6 ± 6.3 | 13.5 ± 17.8* | 10.2 ± 9.9 | 11.8 ± 14.2) |
| Ejection fraction, % | 54.7 ± 10.3 | 52.1 ± 9.1* | 50.5 ± 12.3* | 51.2 ± 11* |
| Left-ventricular EDVI, mL/m² | 66.5 ± 20.6 | 65.3 ± 20.1 | 78.4 ± 28.5* | 71.9 ± 25.5* |
| Residual MVR > moderate | 8 (2.7%) | 5 (2%) | 26 (9.6%)* | 31 (6%)* |
| Technical success | 286 (98.3%) | 247 (99.6%) | 262 (96.7%) | 509 (98.1%) |
| Device success | 284 (97.6%) | 246 (99.2%) | 258 (95.2%) | 504 (97.1%) |
| Procedure success | 283 (97.3%) | 238 (96%) | 253 (93.4%)* | 491 (94.6%) |
| All-cause death | 1 (0.4%) | 4 (1.6%) | 6 (2.2%) | 10 (1.9%) |
| Cardiovascular death | 1 (0.4%) | 4 (1.6%) | 5 (1.9%) | 9 (1.7%) |
| Stroke | 12 (4.1%) | 9 (3.6%) | 4 (1.5%) | 13 (2.5%) |
| Acute myocardial infarction | 1 (0.4%) | 0 | 1 (0.4%) | 1 (0.2%) |
| Reintervention Rate | 8 (2.7%) | 10 (4%)* | 7 (2.6%) | 17 (3.3%)* |
| Data are presented as mean ± SD or n (%). *P < 0.05 at independent t-test between the two periods. EDVI: end-diastolic volume-index; ICU: intensive care unit; MVR: mitral valve regurgitation; PASP: pulmonary artery systolic pressure; SD: standard deviation; TMVT: transcatheter-mitral-valve-technologies. | ||||